Eye Surgery Options: Understanding Your Treatment Choices
Eye surgery encompasses a wide range of procedures designed to treat various conditions affecting vision and eye health. From addressing refractive errors to managing complex retinal conditions, modern ophthalmic surgery offers solutions that can often significantly improve quality of life. Understanding the different types of eye surgeries, their purposes, and what to expect can help patients make informed decisions about their eye care.
Types of Eye Surgery Procedures
Cataract Surgery
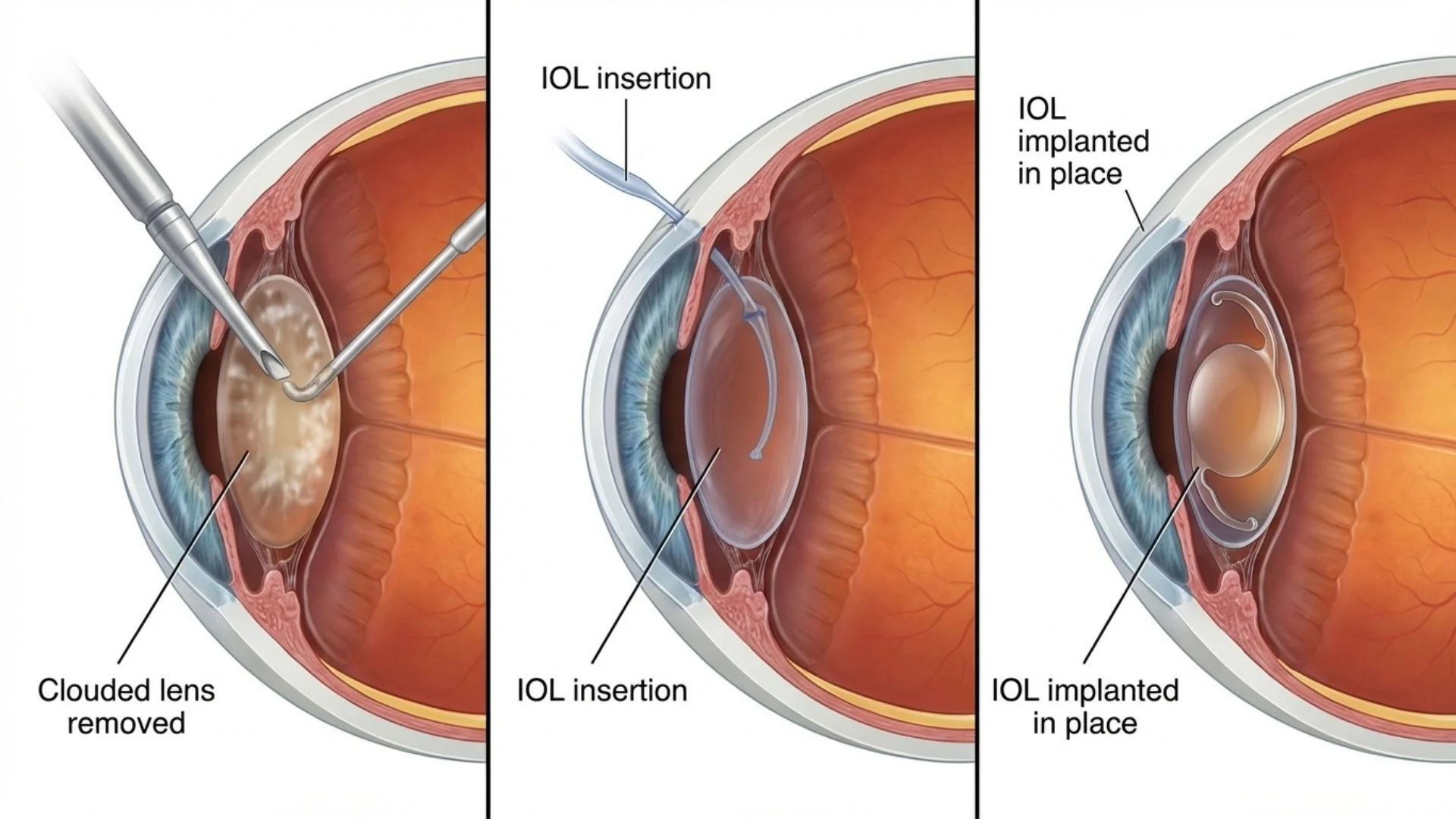
Cataract surgery involves removing the clouded natural lens and replacing it with an artificial intraocular lens. This procedure addresses cataracts, which cause the eye's lens to become opaque over time, resulting in blurred or cloudy vision.
Cataract surgery is the most frequently performed major surgery worldwide, with over 28 million procedures performed annually.
The procedure typically uses small incisions at the edge of the cornea, through which the surgeon removes the clouded lens using a process called phacoemulsification. An artificial lens is then implanted to restore clear vision. Patients usually experience improvement within a few days of surgery, though complete healing may take several weeks.
Cataract surgery is highly successful, with 98–99% of procedures resulting in no major complications. However, potential complications include infection, increased eye pressure, and retinal complications. Some patients may also experience temporary inflammation or corneal swelling during recovery.
Months or years after routine cataract surgery, a condition called after-cataract, posterior capsule opacification, or "secondary cataract" may occur. This happens when residual lens cells grow over the back of the lens capsule, clouding vision months or years after surgery. Posterior capsule opacification affects approximately 20-40% of patients within five years of surgery, but is easily treated with a quick, painless laser procedure called YAG laser posterior capsulotomy.
Retinal Surgery
Retinal surgeries address conditions affecting the light-sensitive tissue at the back of the eye. A vitrectomy removes some or all of the vitreous gel from the eye's centre, treating conditions such as retinal detachment, epiretinal membrane, macular hole, severe diabetic retinopathy with bleeding, and vitreous haemorrhage.
During vitrectomy, surgeons make small incisions to insert fine, specialised instruments that remove vitreous gel and repair retinal damage. The vitreous is replaced with saline solution, gas bubble, or silicone oil to maintain the eye’s structure during healing.
Complications of retinal surgery include infection, bleeding, high or low eye pressure, cataract formation, retinal detachment, and vision loss. Patients receiving gas bubbles must maintain specific head positions for days or weeks and cannot fly until the gas bubble dissipates. Anatomical success rates exceed 90% for many retinal conditions, although visual outcomes vary depending on the extent of pre-existing retinal damage.
Scleral buckling surgery treats retinal detachment by placing a silicone band around the eye to support the retina. This may be combined with vitrectomy for complex cases.
Refractive Surgery
Refractive surgeries modify incoming light rays so that they focus directly on the retina, correcting vision problems such as myopia (short-sightedness), hyperopia (far-sightedness), and astigmatism. Several techniques are available, each with specific indications.
LASIK involves creating a corneal flap, reshaping the underlying tissue with an excimer laser, and repositioning the flap. Most patients notice significant vision improvement within 24 hours. PRK removes the corneal epithelium before laser reshaping, making it suitable for patients with thin corneas or dry eyes. Recovery typically takes longer than LASIK, with vision improving over several weeks.
SMILE surgery is a minimally invasive technique that creates a small lens-shaped piece of tissue within the cornea through a tiny incision. This procedure requires no corneal flap and may result in less dry eye compared to LASIK.
While refractive surgeries are generally effective, risks include dry eye, glare, haloes around lights, undercorrection or overcorrection, infection, and rarely, vision loss. Not all patients achieve perfect vision, and some may still require glasses for certain activities.
Glaucoma Surgery
Glaucoma surgery lowers eye pressure to prevent further vision loss from optic nerve damage in individuals with glaucoma. Various procedures address different types of glaucoma, although surgery cannot restore vision already lost due to the disease.
Laser procedures such as selective laser trabeculoplasty and laser iridotomy are performed with numbing drops. Trabeculectomy creates a small opening in the sclera to allow fluid drainage, while glaucoma implant surgery inserts a tiny drainage tube. Minimally invasive glaucoma surgery techniques have emerged as newer options with potentially faster recovery times and fewer complications.
Complications may include infection, bleeding, scarring that blocks the drainage pathway, excessively low eye pressure, cataract formation, and failure to adequately control eye pressure requiring additional procedures.
Corneal Surgery
Corneal transplant surgery replaces diseased or scarred cornea with healthy donor tissue. Depending on which corneal layers are affected, surgeons may replace partial layers or the entire cornea.
Phototherapeutic keratectomy uses laser technology to remove corneal scars, opacities, and dystrophies.
Pterygium excision and conjunctival grafting remove abnormal tissue growth that extends onto the cornea from the conjunctiva.
Risks include graft rejection, infection, irregular astigmatism, glaucoma, and delayed healing. Anti-rejection medications are typically required long-term after corneal transplantation.
Oculoplastic Surgery
Procedures in this category address structures around the eye, including eyelids and tear drainage systems. Blepharoplasty repairs drooping eyelids that impair vision or affect appearance, while tear duct surgery corrects obstruction causing excessive tearing.
How to Prepare for Eye Surgery
Preparation varies by procedure type. Patients typically undergo a comprehensive eye examination, including dilated retinal examination and specialised imaging. Medical history review identifies conditions that may affect surgery or healing, such as diabetes, bleeding disorders, or medications requiring adjustment.
Most procedures require fasting before surgery. Patients should arrange transportation home, as vision may be temporarily impaired and driving unsafe.
Anaesthesia Options for Eye Surgery
Many eye surgeries use topical anaesthesia eye drops or local anaesthesia blocks, allowing patients to remain awake while preventing pain. This enables patients to maintain the still, flat position necessary for delicate eye surgery. General anaesthesia may be used for children, patients who are unable to cooperate, or certain long and complex procedures.
Eye Surgery Recovery: What to Expect
Recovery timelines vary significantly. Some patients notice improvement within hours, while others require weeks or months for optimal results. Temporary symptoms often include eye discomfort, light sensitivity, tearing, and blurry vision. Prescribed eye drops prevent infection and reduce inflammation during healing.
Activity restrictions may include avoiding heavy lifting, swimming, or rubbing the eyes. Follow-up appointments monitor healing progress and address complications promptly.
Risks and Considerations for Eye Surgery
Eye surgery outcomes depend on multiple factors, including the specific condition being treated, pre-existing eye health, surgical technique, and individual healing responses. While modern surgical techniques have high success rates, no procedure guarantees perfect results or is entirely risk-free.
Patients should discuss realistic expectations, potential complications, alternative treatments, and long-term outcomes with their ophthalmologist. Understanding both benefits and limitations enables informed decision-making about vision care.
Medical Disclaimer: This article provides general information about eye surgeries and should not replace professional medical advice. Each patient's situation is unique, and treatment recommendations should be made by qualified healthcare providers after a comprehensive evaluation. If you are experiencing vision problems or considering eye surgery, please consult an ophthalmologist to discuss your specific needs and treatment options.















