Cataracts are one of the most common age-related treatable causes of vision loss, affecting millions of people worldwide. Although the prospect of surgery may seem daunting, modern cataract surgery has evolved into one of the safest and most successful procedures in healthcare. Understanding when to proceed with cataract surgery involves more than simply documenting the impact of cataract on the vision, more specifically visual acuity. Contemporary clinical practice emphasises functional impairment, quality of life impact, and individualised decision-making rather than relying only on rigid numerical thresholds of visual acuity.
Understanding Cataract Development and Progression
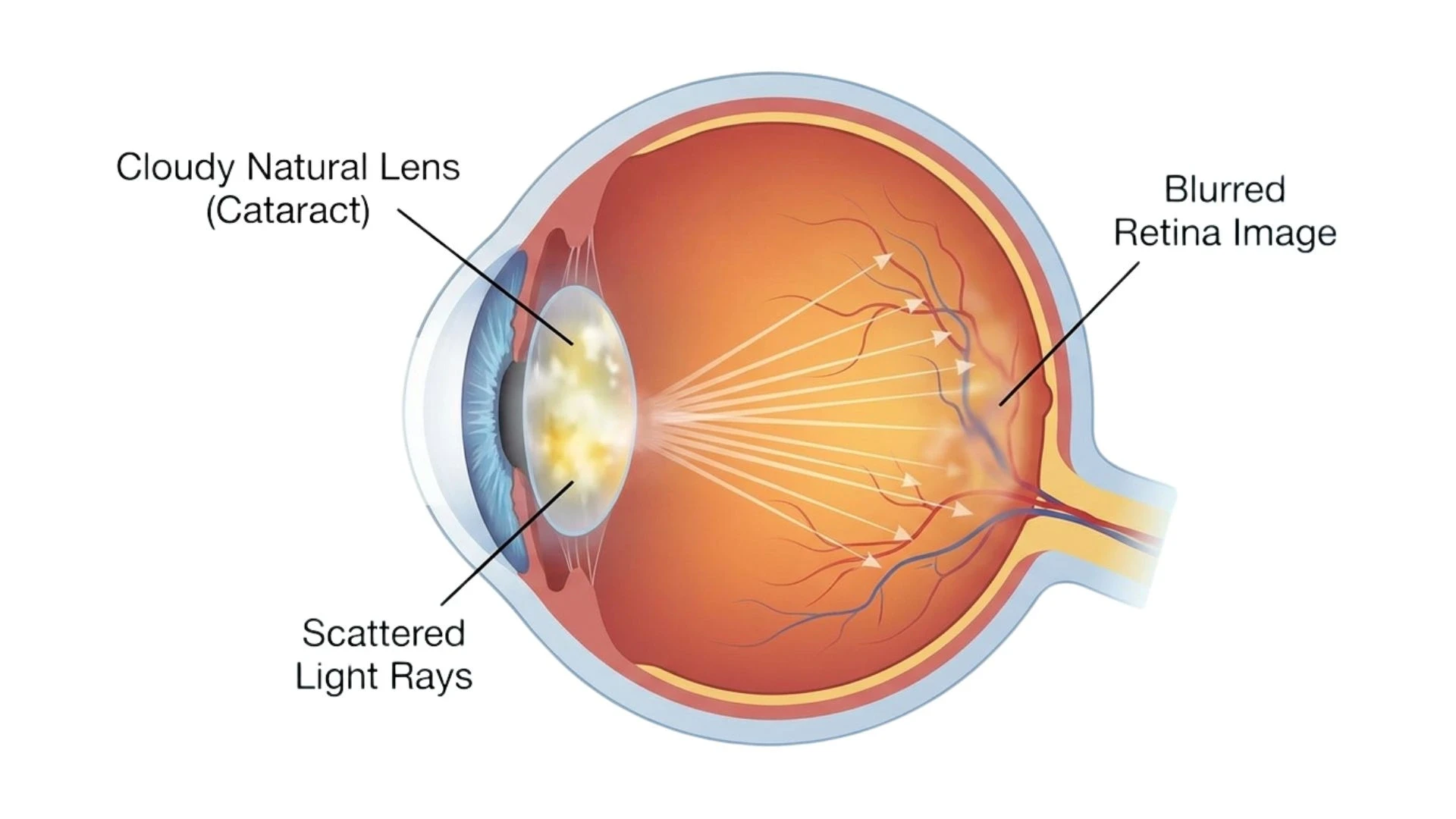
A cataract occurs when the normally clear natural lens inside your eye gradually becomes cloudy, scattering light and reducing the quality of images reaching your retina. This progressive condition typically develops over months to years, with symptoms ranging from subtle blurring to severe visual disability. Age is the primary risk factor, though other contributors include diabetes, prolonged corticosteroid medication use, eye injuries, cigarette smoking and certain genetic factors.
Moving Beyond Visual Acuity: The Modern Approach to Surgical Timing
The question facing patients and eye surgeons is not whether cataracts will eventually require treatment, but when surgery will provide meaningful benefit. Modern guidelines have moved away from the outdated practice of waiting until cataracts are "ripe" before considering a surgical intervention.
Contemporary clinical guidelines have abandoned rigid visual acuity thresholds in favour of a patient-centred framework. The European Society of Cataract and Refractive Surgeons (ESCRS) emphasises that surgical indications should include visual acuity and function, subjective visual disability, and expected benefit, without mandating specific numerical cut-offs of visual acuity. The Royal Australian and New Zealand College of Ophthalmologists (RANZCO) states explicitly that there is no visual acuity level above or below which surgery is or is not indicated.
The Australian Cataract Clinical Care Standard, updated in 2025, defines surgical candidacy as the presence of lens opacity that limits vision-related activities and causes clinically significant visual impairment through reduced best-corrected visual acuity, disabling glare, or contrast sensitivity loss.
Key Indicators That Surgery May Be Appropriate
Functional Impairment in Daily Activities
While cataract surgery is an elective planned procedure, the decision to consider surgery has to be individualised for each patient. The most important consideration in surgical timing is how cataracts affect your ability to perform activities that matter to you. Important functional areas include difficulty with reading (particularly fine print or in dim lighting), recognising faces, watching television, safe mobility (especially navigating stairs), driving (particularly at night), and performing work tasks requiring visual precision. When cataracts interfere with these activities, surgery becomes a reasonable consideration.
Symptomatic Visual Disturbances
Beyond simple blurring of vision, cataracts produce characteristic symptoms that may impact quality of life. Disabling glare is one of the most common complaints, with patients describing overwhelming sensitivity to bright lights, difficulty with oncoming headlights when driving, and inability to see in bright sunlight despite wearing sunglasses.Reduced contrast sensitivity appears as difficulty distinguishing objects from their background generally described as "washed out" vision that spectacles cannot correct. Some patients experience double images (monocular diplopia) or bothersome halos around lights, particularly noticeable during night driving. These symptoms often respond well to cataract surgery, even when standard visual acuity measurements suggest only modest impairment.
Impact on Quality of Life
Surgical decision-making increasingly incorporates the overall effect of a cataract on the quality of life recognising that no single clinical test fully captures the impact of cataract-associated vision loss.
Cataracts can impact mental health and psychological wellbeing through frustration with declining abilities, anxiety about deterioration, limited social participation and independence, social isolation and overall life satisfaction. According to the World Health Organization, the visual impairment from a cataract also increases the risk of falls and the associated comorbidities.
Factors That May Influence Surgical Timing
Presence of Other Eye Conditions
Concurrent eye conditions require special consideration when planning cataract surgery. Patients with macular degeneration, diabetic retinopathy, glaucoma, or other retinal diseases may still benefit from cataract removal, though final visual outcomes depend partly on the severity of coexisting conditions.Modern guidelines encourage individualised timing in such cases, often recommending surgery when underlying disease is stable and aligned with the patient's functional needs.
Fellow Eye Status
When one eye has significantly better vision than the other, the risk-benefit calculation for operating on the better eye requires careful consideration. Modern cataract surgery carries very low risk (serious vision loss occurs in well under 1% of procedures), but the consequences of an adverse outcome in a patient's only functional eye need thorough discussion.
When to Seek Consultation with an Eye Specialist
If you are experiencing progressive difficulty with activities you previously managed comfortably, troublesome glare that spectacles do not alleviate, declining vision despite updated prescriptions, or concerns about how your vision is affecting your independence, a comprehensive cataract assessment may be appropriate.
A comprehensive evaluation includes detailed visual function assessment, measurement of how cataracts affect your daily activities, thorough examination of your eye health including retinal evaluation, advanced biometry and intraocular lens (IOL) power calculations, and discussion of surgical timing, techniques, and lens options tailored to your needs.
The Decision-Making Process: A Collaborative Approach
The decision about when to proceed with cataract surgery should emerge from discussion between you and your ophthalmologist, considering the degree of visual impairment, impact on quality of life, your visual needs based on lifestyle, realistic expectations about outcomes, individual risk factors, and personal preferences regarding spectacle dependence.There is no universally "correct" time for cataract surgery. Some patients benefit from earlier intervention when cataracts interfere with important activities, whilst others may reasonably defer surgery when visual impairment remains mild. The key is ensuring the decision reflects your individual circumstances rather than arbitrary thresholds.
Taking the Next Step
If cataracts are affecting your vision and quality of life, we encourage you to schedule a comprehensive evaluation. Contact our clinic today to book your cataract consultation. Together, we can determine the optimal timing and approach to restore clear, comfortable vision and help you maintain your independence and quality of life.






