Vitreoretinal Surgery
Vitreoretinal surgery encompasses a range of delicate procedures performed on the vitreous gel and retina at the back of the eye. These surgeries address serious conditions that can threaten vision, including retinal detachment, macular holes, and complications from diabetic eye disease.
Understanding the Procedure
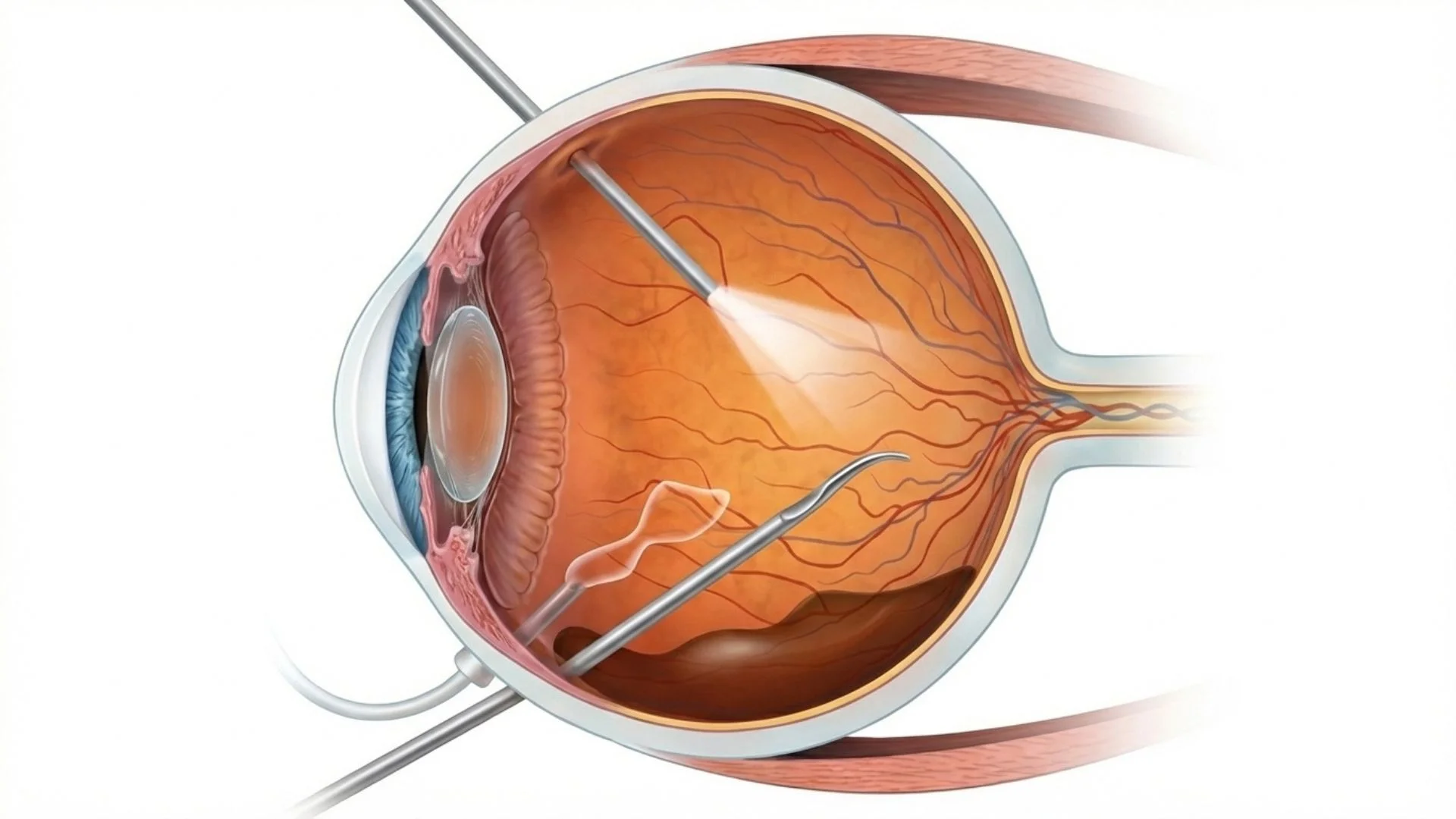
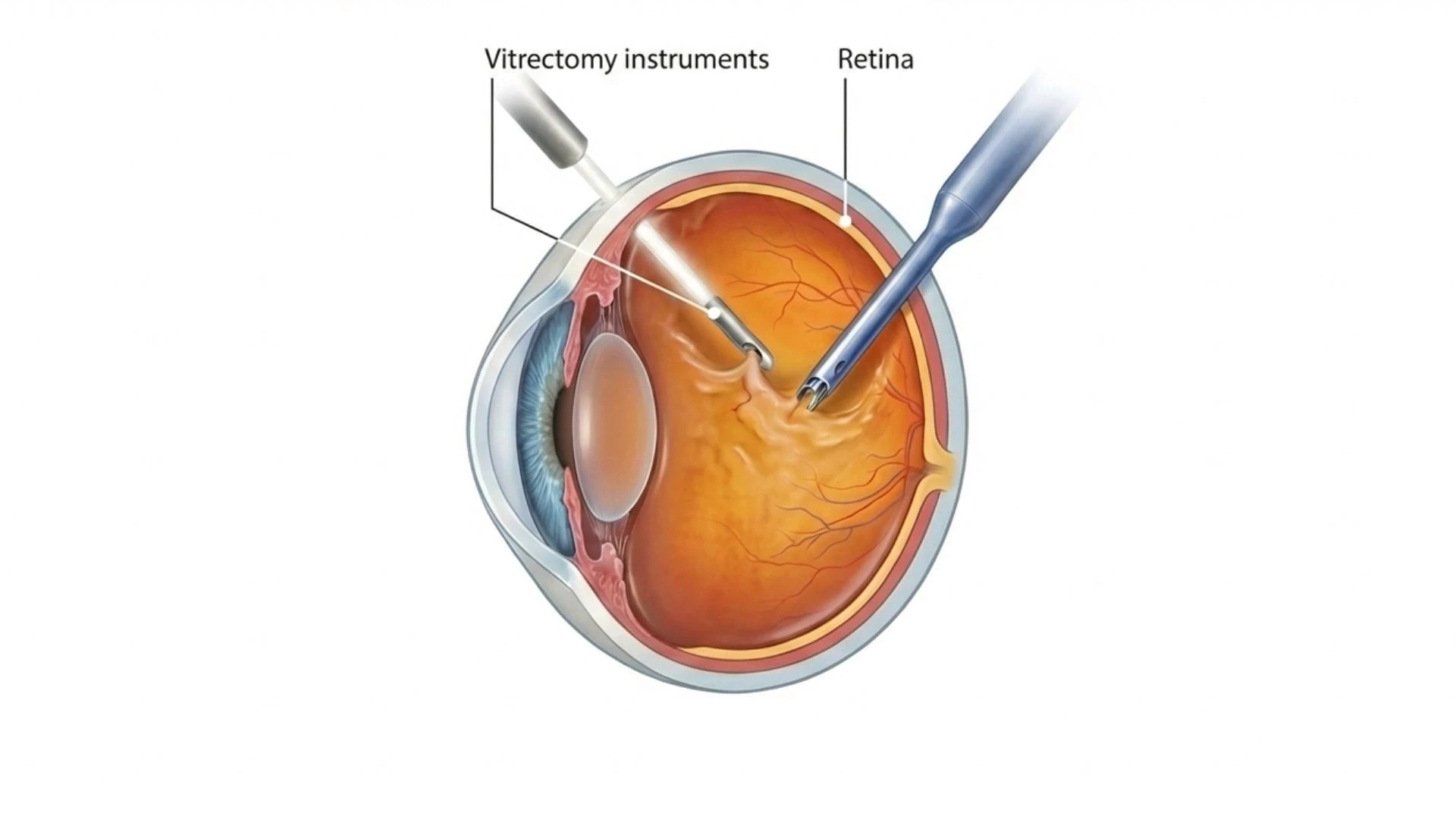
The most common vitreoretinal procedure is vitrectomy, which involves removing the vitreous gel-the clear, jelly-like substance filling the eye's interior. This allows the surgeon access to repair the retina, remove scar tissue, or address other abnormalities.
Modern vitrectomy uses very fine instruments inserted through tiny incisions (typically 0.5mm or less). The National Eye Institute provides comprehensive information on retinal conditions that may require surgical intervention.
Conditions Treated
Vitreoretinal surgery may be recommended for:
Retinal detachment where the retina separates from its supporting tissue
Macular hole a small break in the central retina affecting detailed vision
Epiretinal membrane scar tissue on the retinal surface causing distortion
Vitreous haemorrhage bleeding into the vitreous cavity
Complications of diabetic retinopathy including tractional detachment
Severe eye injuries affecting the vitreous or retina
Dislocated intraocular lens following previous eye surgery
Surgical Approaches
Several techniques may be used depending on the specific condition:
Vitrectomy removes vitreous gel and allows direct treatment of retinal problems. The vitreous is replaced with saline solution, a gas bubble, or silicone oil to help hold the retina in position during healing.
Scleral buckle involves placing a silicone band around the eye's exterior to gently push the eye wall toward the detached retina.
Pneumatic retinopexy uses an injected gas bubble combined with laser or freezing treatment for certain types of retinal detachment.
Your surgeon will recommend the most appropriate approach based on your specific condition.
What to Expect
Vitreoretinal surgery is typically performed as a day procedure under local anaesthesia, though some complex cases may require general anaesthesia:
Procedure duration varies from 30 minutes to several hours depending on complexity
You may need to maintain a specific head position after surgery if a gas bubble is used
The American Academy of Ophthalmology notes that positioning requirements are crucial for successful outcomes in certain procedures
Potential Risks
Vitreoretinal surgery is performed to address serious sight-threatening conditions. Patients should understand:
Cataract formation is common in patients who have not had previous cataract surgery, often developing within one to two years
Raised eye pressure may occur temporarily or require ongoing management
Re-detachment of the retina occurs in approximately 10-15% of cases, possibly requiring further surgery
Infection is rare but serious
Bleeding may occur during or after surgery
Vision may not fully recover depending on the condition's severity and how long it was present before treatment
The goal of surgery is often to prevent further vision loss and stabilise the condition, rather than restore vision to normal levels.
Recovery
Recovery from vitreoretinal surgery is gradual and requires patience:
If a gas bubble is used:
Vision will be very poor initially as you look through the bubble
The bubble gradually shrinks and is absorbed over weeks (timing depends on gas type)
You must not fly or travel to high altitude until the gas has completely absorbed-this is critical for your safety
Specific head positioning may be required for days to weeks
General recovery:
Vision typically improves gradually over weeks to months
Final visual outcome may not be apparent for three to six months
Some permanent changes in vision, peripheral field, or night vision may persist
Medical Disclaimer: This information provides general guidance about vitreoretinal surgery and should not replace professional medical advice. These procedures address serious eye conditions, and outcomes depend on many factors including the specific condition, its duration, and individual healing responses. All surgical procedures carry risks. Please consult with our ophthalmologists for a thorough evaluation and discussion of your particular situation.
Seek immediate attention if you experience: Severe pain, sudden decrease in vision, increasing redness, or new flashes and floaters.