Glaucoma Surgery
Glaucoma surgery creates new drainage pathways to lower eye pressure when medications and laser treatments are insufficient. These procedures aim to protect remaining vision by reducing pressure on the optic nerve.
Understanding Glaucoma Surgery
Glaucoma damages the optic nerve, typically due to elevated eye pressure. When conservative treatments cannot adequately control pressure, surgery may be recommended to create alternative routes for fluid to drain from the eye.
The National Eye Institute emphasises that while glaucoma surgery cannot restore lost vision, it can help prevent further damage.
Types of Glaucoma Surgery
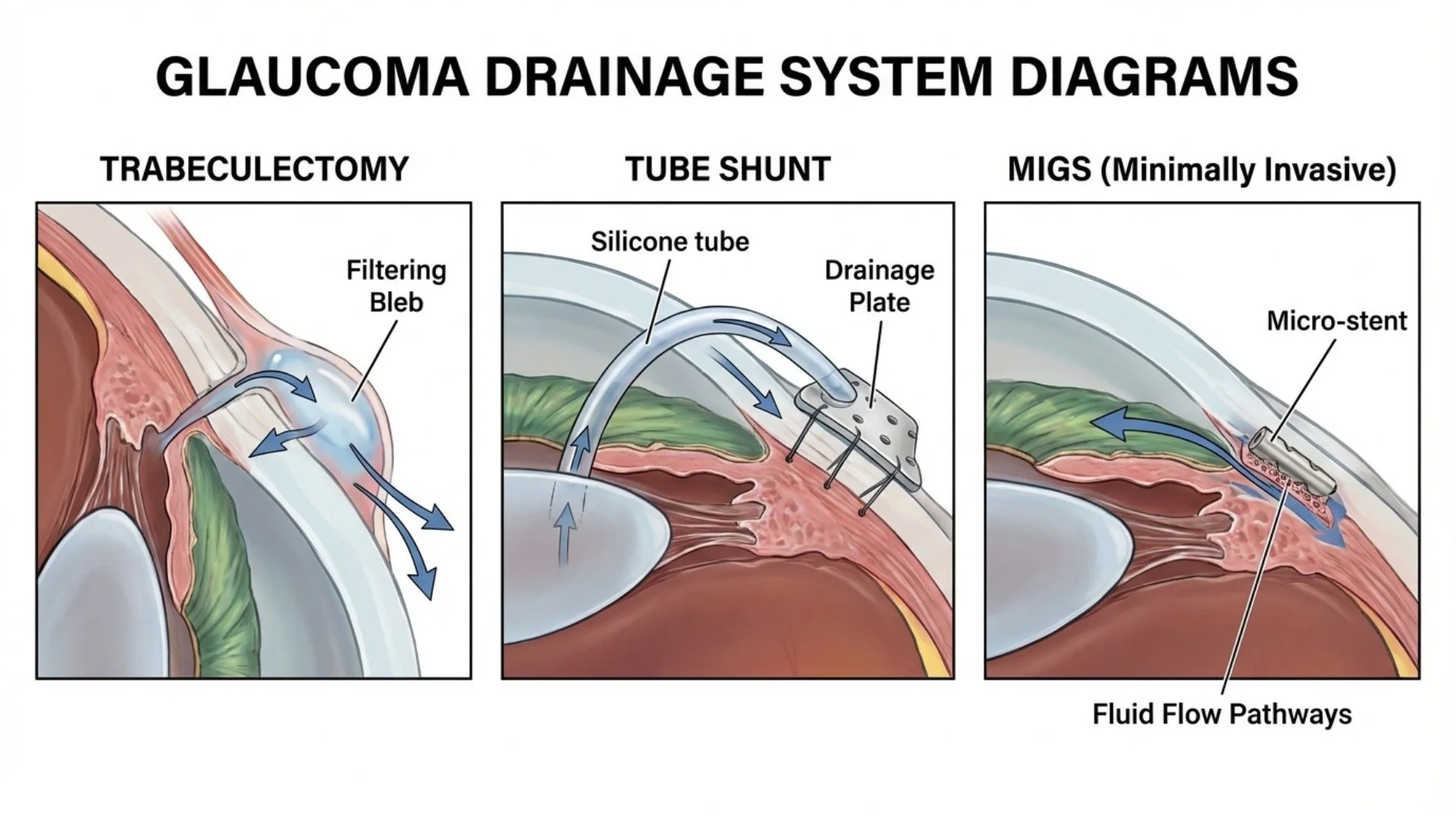
Trabeculectomy creates a small flap in the sclera (white of the eye) that allows fluid to drain into a pocket beneath the conjunctiva, where it is absorbed. This has been the traditional approach for many years.
Glaucoma Drainage Devices (tube shunts) involve placing a small tube that channels fluid to a plate positioned on the eye surface, creating an alternative drainage pathway.
Minimally Invasive Glaucoma Surgery (MIGS) encompasses newer procedures that work through tiny incisions, often performed during cataract surgery. These include:
Devices that improve drainage through the eye's natural outflow pathways
Tiny stents placed in the drainage angle
Small shunts that create new drainage routes
Who May Need Surgery
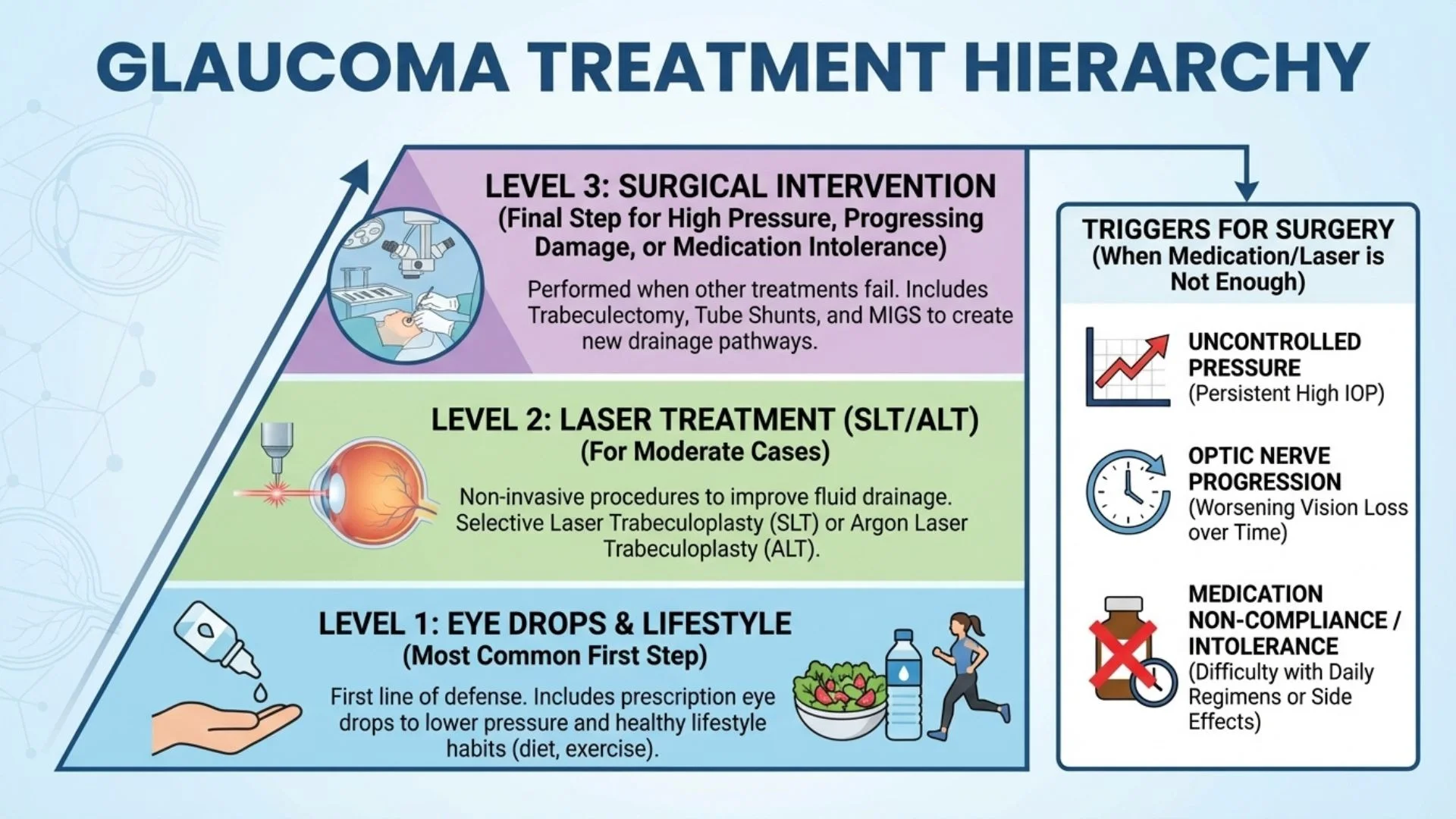
Glaucoma surgery may be recommended when:
Eye pressure remains too high despite maximum medication
Glaucoma continues to progress on current treatment
Side effects make medications difficult to tolerate
Adherence to complex drop regimens is challenging
The type or severity of glaucoma requires more aggressive treatment
The American Academy of Ophthalmology provides detailed information about surgical options for glaucoma.
What Results Can Be Expected
The goal of glaucoma surgery is to lower eye pressure sufficiently to slow or halt optic nerve damage:
Trabeculectomy and tube shunts can achieve significant pressure reduction
Success rates vary depending on the type of glaucoma and individual factors
Some patients may still require medications after surgery, though often fewer
MIGS procedures typically achieve more modest pressure reduction but with faster recovery
Important to understand:
Surgery protects remaining vision but cannot restore what has been lost
Ongoing monitoring is essential-glaucoma requires lifelong care
The surgical opening may scar over time, reducing effectiveness
Potential Risks
Glaucoma surgery carries risks that must be weighed against the risk of vision loss from uncontrolled glaucoma:
Infection is a serious risk requiring prompt treatment
Bleeding inside the eye
Pressure that is too low (hypotony) can affect vision
Cataract development or progression
Scarring that reduces the effectiveness of the drainage
Need for additional surgery if the initial procedure is insufficient
Vision loss can occur, though the surgery aims to prevent this
MIGS procedures generally have fewer serious risks but may be less effective at lowering pressure.
Recovery varies: Traditional surgery (trabeculectomy, tubes) requires more intensive follow-up than MIGS. Your surgeon may need to perform minor adjustments in the weeks after surgery.
Medical Disclaimer: This information provides general guidance about glaucoma surgery and should not replace professional medical advice. Glaucoma is a complex condition, and the most appropriate surgical approach depends on many individual factors. Surgery carries risks and does not guarantee prevention of further vision loss. Please consult with our glaucoma specialists for a thorough evaluation and discussion of your treatment options.
Seek immediate attention if you experience: Severe pain, sudden vision decrease, increasing redness, or any signs of infection.

