Many people notice tiny specks, strands, or cobweb-like shapes drifting across their vision, or brief flashes of light at the edge of their sight. These visual symptoms are called eye floaters and flashes, and while they are often harmless age-related changes, they can also signal a serious retinal problem such as a retinal tear or retinal detachment. Understanding the difference between benign symptoms and an eye emergency helps you seek timely care from a retina specialist in Singapore and protect your long-term vision health.
What Are Eye Floaters?
Eye floaters are small shapes that move with your eye movements and seem to drift when you try to look directly at them. They appear as dark spots, squiggly lines, cobweb-like strands, or small rings, most visible against bright backgrounds like a blue sky or white wall.
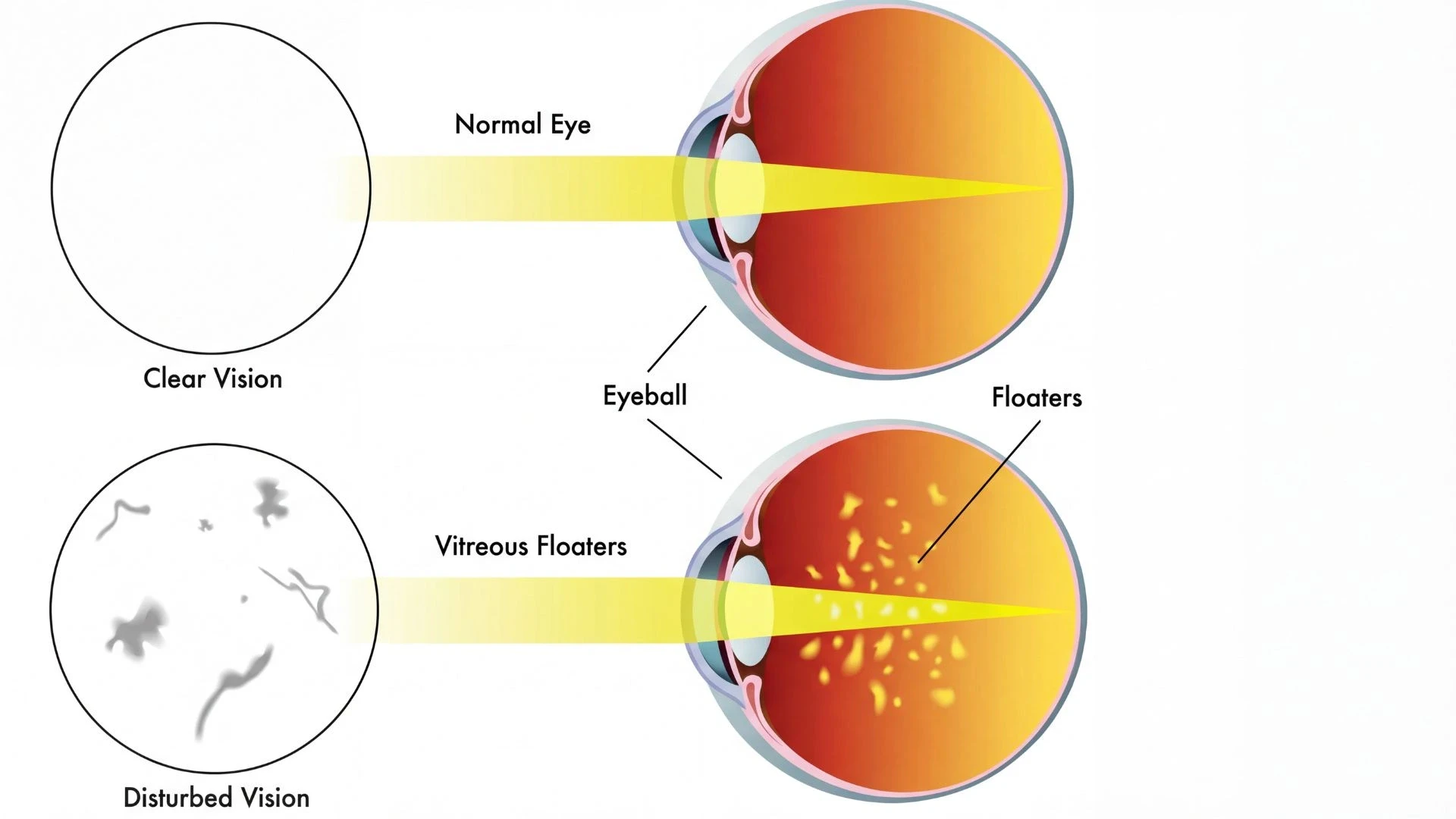
Floaters form when tiny clumps of gel or cells develop inside the vitreous, the clear, jelly-like substance filling the back of the eye. As the vitreous shrinks and liquefies with age, it can pull away from the retina and create shadows; these shadows are perceived as floaters.
For comprehensive patient education on floaters and flashes, the American Academy of Ophthalmology provides detailed information on causes, symptoms, and when to seek care.
Common Causes of Eye Floaters
Most floaters are related to natural vitreous aging and don't threaten sight. However, floaters may also indicate:
Posterior Vitreous Detachment (PVD)
Retinal tears or detachment
Eye inflammation (uveitis)
Previous eye surgery or trauma
Diabetic retinopathy complications
A sudden onset or marked increase in floaters should be evaluated promptly by an eye specialist in Singapore.
What Causes Flashes in Your Vision?
Flashes of light in vision, also known as photopsia, appear as brief flickers, lightning streaks, or camera flashes at the edge of your visual field. They occur when the vitreous gel tugs on the light-sensitive retina, stimulating it mechanically and causing the brain to interpret this pull as light. Persistent or recurrent new flashes, especially combined with new floaters, can indicate that the vitreous is pulling strongly on the retina and that a retinal tear or retinal detachment may be developing.
The National Eye Institute offers authoritative guidance on recognizing warning signs requiring urgent medical assessment.
When Flashes and Floaters Appear Together
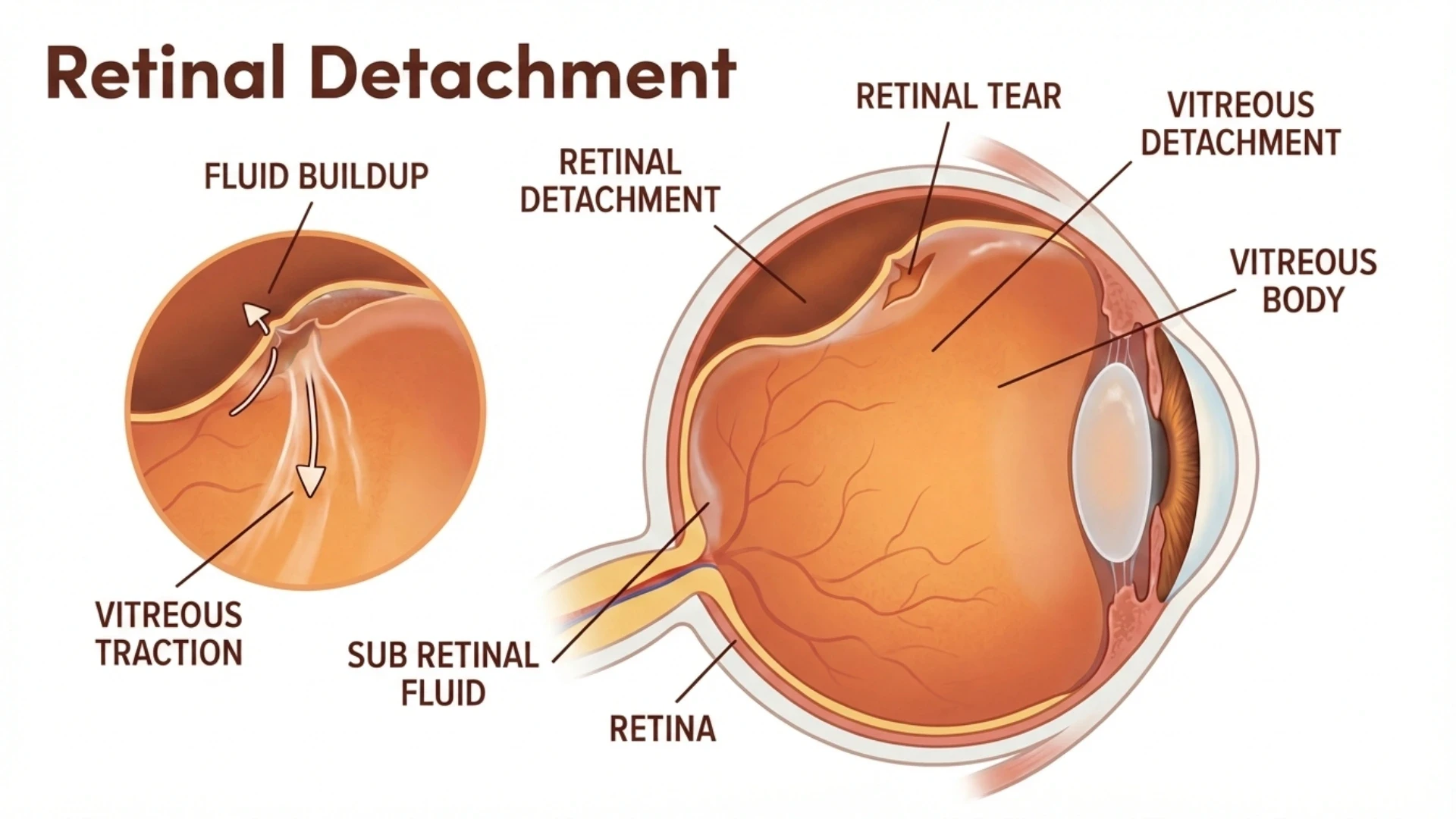
Flashes and floaters often appear together during Posterior Vitreous Detachment. In many cases, PVD is a normal aging process where the vitreous separates cleanly from the retina without damage. However, strong vitreous traction can create a retinal tear, allowing fluid to accumulate behind the retina, potentially leading to retinal detachment.
Understanding Retinal Tears and Retinal Detachment
What Is Posterior Vitreous Detachment (PVD)? :
Posterior Vitreous Detachment is a common age-related eye condition where the vitreous gel shrinks and pulls away from the retina. Many people over age 50 develop PVD. In most cases, it causes only floaters and occasional flashes, with the retina remaining intact.
Because PVD and retinal tears produce similar symptoms, examination by an ophthalmologist in Singapore is essential to distinguish between benign PVD and a potential retinal emergency.
How Retinal Tears Form :
If the vitreous pulls too firmly on thin or weak retina, it creates a small break or tear. A retinal tear allows fluid to seep through and collect behind the retina—the critical step that can progress to retinal detachment if untreated. Retinal tears can often be managed with clinic-based laser photocoagulation or cryotherapy when detected promptly.
Understanding Retinal Detachment: An Eye Emergency
A retinal detachment occurs when fluid accumulates behind the retina and lifts it away from the back wall of the eye. Once detached, the retina loses its blood supply and oxygen, placing vision at serious risk. Retinal detachment is an ophthalmic emergency requiring surgery to prevent permanent vision loss.
Common retinal detachment symptoms include:
A dark curtain or veil moving across vision
A shadow in peripheral vision that gradually enlarges
Sudden blurry or distorted central vision
Decreased visual acuity in one eye
The Royal College of Ophthalmologists provides comprehensive patient information on retinal detachment symptoms and treatment.
Retinal Detachment Warning Signs: When to See a Specialist Immediately
Seek urgent care at a retina centre in Singapore if you experience:
Sudden onset or rapid increase in eye floaters, especially a "shower" of black spots
New or repeated flashes of light, particularly at the edge of vision
A dark curtain, veil, or shadow moving across vision
Sudden blurry vision or noticeable drop in visual clarity
Loss of peripheral vision that progressively worsens
Early diagnosis enables retinal tear treatment before the retina fully detaches.
Who Is at Higher Risk of Retinal Detachment?
High Myopia (Short-Sightedness) and Risk :
High myopia is particularly prevalent in Singapore, with Southeast Asia having among the highest myopia rates globally. In highly myopic eyes, the elongated eyeball stretches and thins the retina, making it vulnerable to tears and detachment. People with high myopia (above -6.00 diopters) face significantly higher retinal detachment risk.
Other Risk Factors
Key retinal detachment risk factors include:
Age over 50 years
Previous cataract surgery
Previous retinal detachment in the other eye
Significant eye trauma
Family history of retinal detachment
Lattice degeneration (peripheral retinal thinning)
The American Society of Retina Specialists explains risk factors in detail for patient education.
Diagnosis at a Retina Specialist in Singapore
During comprehensive retinal evaluation, the retina specialist or ophthalmologist will:
Take detailed medical history of symptoms
Check visual acuity and intraocular eye pressure
Administer dilating eye drops for thorough retinal examination
Examine vitreous and retina using specialized microscopes and lenses
Additional imaging may include:
Optical Coherence Tomography (OCT): Cross-sectional retinal images
B-scan ultrasound: When retina cannot be viewed directly
Fundus photography: Documents retinal appearance
These steps distinguish simple PVD from serious problems like retinal tears or detachment.
Treatment Options for Retinal Tears and Detachment
Clinic-Based Retinal Tear Treatment
If a retinal tear is detected before detachment, it can often be sealed with outpatient procedures:
Laser Photocoagulation: Creates small burns around the tear, forming a scar that "welds" the retina to underlying tissue. Success rate: 90-95% when performed early.
Cryotherapy: Uses a freezing probe applied to the eye's exterior to seal the tear. Preferred when tears are at far periphery or laser is unsuitable.
These treatments significantly reduce retinal detachment risk when applied early.
Surgical Options for Retinal Detachment
If retinal detachment has occurred, surgery is usually required:
Pneumatic Retinopexy:
Gas bubble injection to press retina back
Combined with laser or cryotherapy
Requires specific head positioning
Success rate: 60-80%
Scleral Buckle Surgery:
Silicone band placed around eye wall
Indents eye to counteract traction
Success rate: 80-90%
Permanent implant
Vitrectomy:
Surgical vitreous gel removal
Retina flattened and reattached
Gas or silicone oil injected
Success rate: 85-95%
Most versatile for complex detachments
Each option has specific benefits, limitations, and potential complications including cataract formation, elevated eye pressure, or need for additional procedures. The National Eye Institute provides detailed information on treatment options.
Protecting Your Vision: Prevention Tips
Regular Eye Examinations :
Schedule annual dilated examinations with an ophthalmologist
High myopia patients: examinations every 6-12 months
After age 60: increase frequency as recommended
Recognize Warning Symptoms :
Learn retinal detachment symptoms early
Seek same-day assessment for sudden floaters, flashes, or vision loss
Keep emergency contact information accessible
Eye Protection:
Wear protective eyewear during sports and high-risk activities
Use safety glasses for occupational hazards
Prevent eye trauma through proper precautions
Early recognition and timely treatment at a retina centre in Singapore can preserve vision and reduce permanent sight loss risk.
Expert Retina Care at International Eye Cataract Retina Centre
International Eye Cataract Retina Centre provides comprehensive retinal care at Mount Elizabeth Medical Centre and Farrer Park Medical Centre, Singapore.
Services include:
Emergency same-day consultations
Comprehensive dilated retinal examinations
Laser photocoagulation and cryotherapy
Advanced surgical options: vitrectomy, scleral buckle, pneumatic retinopexy
High myopia retinal screening
If you've noticed new floaters, flashes, or curtain effect in vision, arrange a consultation with an eye specialist in Singapore for thorough evaluation.
Frequently Asked Questions
How common is retinal detachment in Singapore? Retinal detachment affects approximately 1 in 10,000 people annually. Singapore's high myopia prevalence means local rates may exceed global averages.
Can retinal detachment be prevented? While not all cases are preventable, early treatment of retinal tears prevents progression. Regular eye examinations enable early detection.
What is recovery time after surgery? Recovery varies: pneumatic retinopexy requires 1-2 weeks restricted activity; vitrectomy or scleral buckle needs 2-4 weeks. Full visual recovery can take 3-6 months.
Will vision return to normal? Visual outcomes depend on detachment extent, macula involvement, treatment timing, and surgical success. Many patients regain functional vision, though complete recovery isn't always possible.
Important Medical Disclaimer
This article provides general educational information about flashes, floaters, and retinal detachment in Singapore. It is not personalized medical advice and should not replace consultation with a qualified ophthalmologist or retina specialist.
If you experience sudden vision changes, new flashes and floaters, or a curtain over your sight, seek prompt medical assessment immediately. Retinal detachment is a time-sensitive emergency where treatment delays can cause permanent vision loss.
Additional Resources
For further authoritative information:






