Retina: Understanding Your Eye's Visual Processing Center
The retina is a thin layer of light-sensitive tissue located at the back of your eye that plays a role in vision. Think of it as the film in a traditional camera or the sensor in a digital camera-it captures the light that enters your eye and converts it into signals that your brain can understand as images. This delicate structure, no thicker than a sheet of paper, contains millions of specialized cells that work together to help you see the world around you, from reading text on your phone to recognizing faces across a room. When the retina experiences damage or disease, it can significantly affect your ability to see clearly, making understanding retinal health important for maintaining quality of life.
Important: All retinal treatments and procedures carry risks. This information is educational and should not replace individual consultation with a qualified ophthalmologist.
Understanding the Retina
The retina is a complex, multi-layered tissue that lines the inside back wall of your eyeball. Measuring approximately 0.5 millimetres in thickness, this remarkable structure contains over 100 million light-sensitive cells that work continuously to process visual information. The retina forms part of the eye's middle layer, called the uvea, and is connected directly to your brain through the optic nerve.
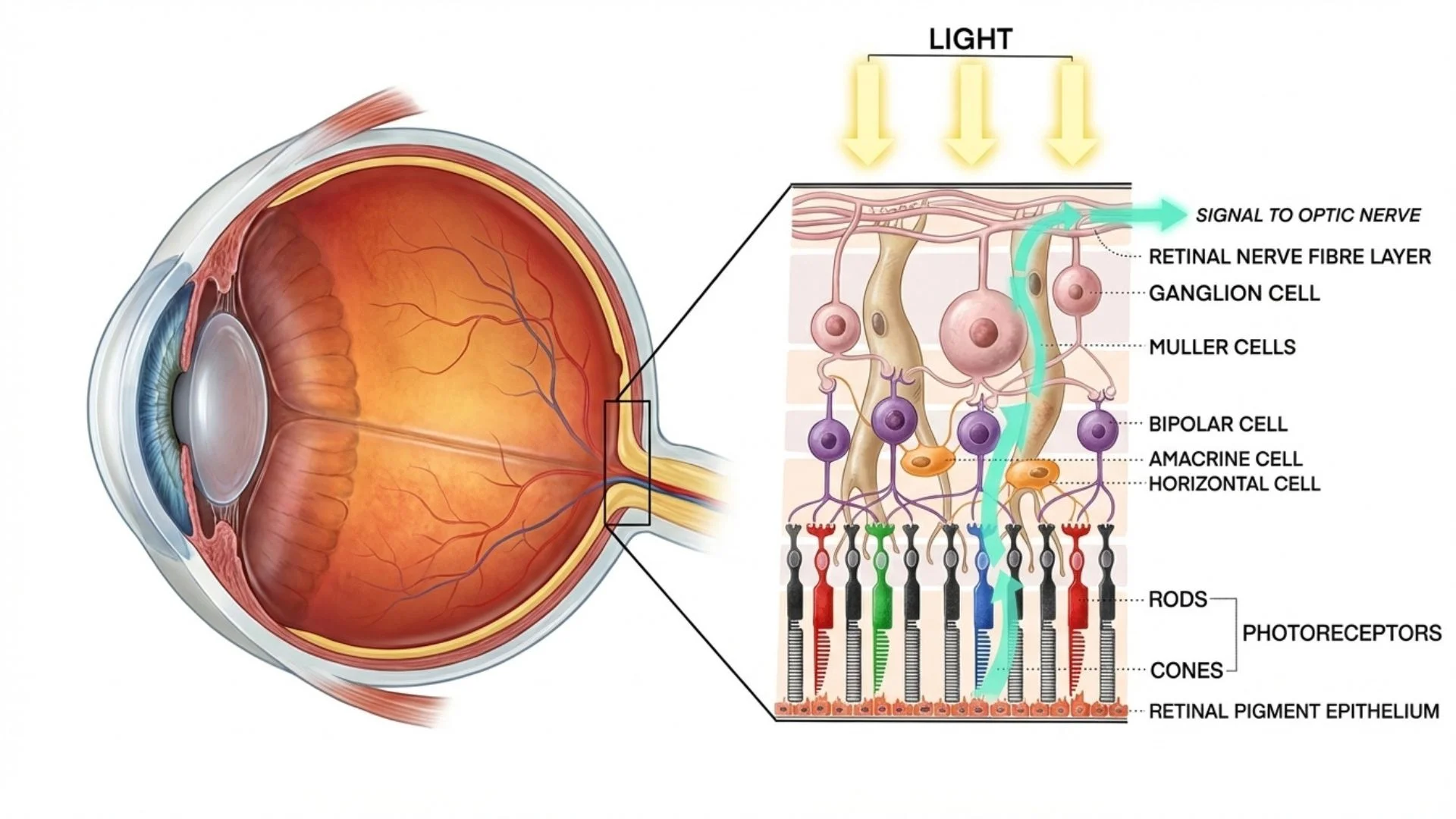
When light enters your eye, it first passes through the cornea and lens, which focus the light rays onto the retina. The retina then converts these light rays into electrical impulses that travel through the optic nerve to your brain, where they are interpreted as the images you see. This process happens instantaneously and continuously throughout your waking hours, allowing you to navigate your environment and interact with the world.
Anatomy and Structure of the Retina
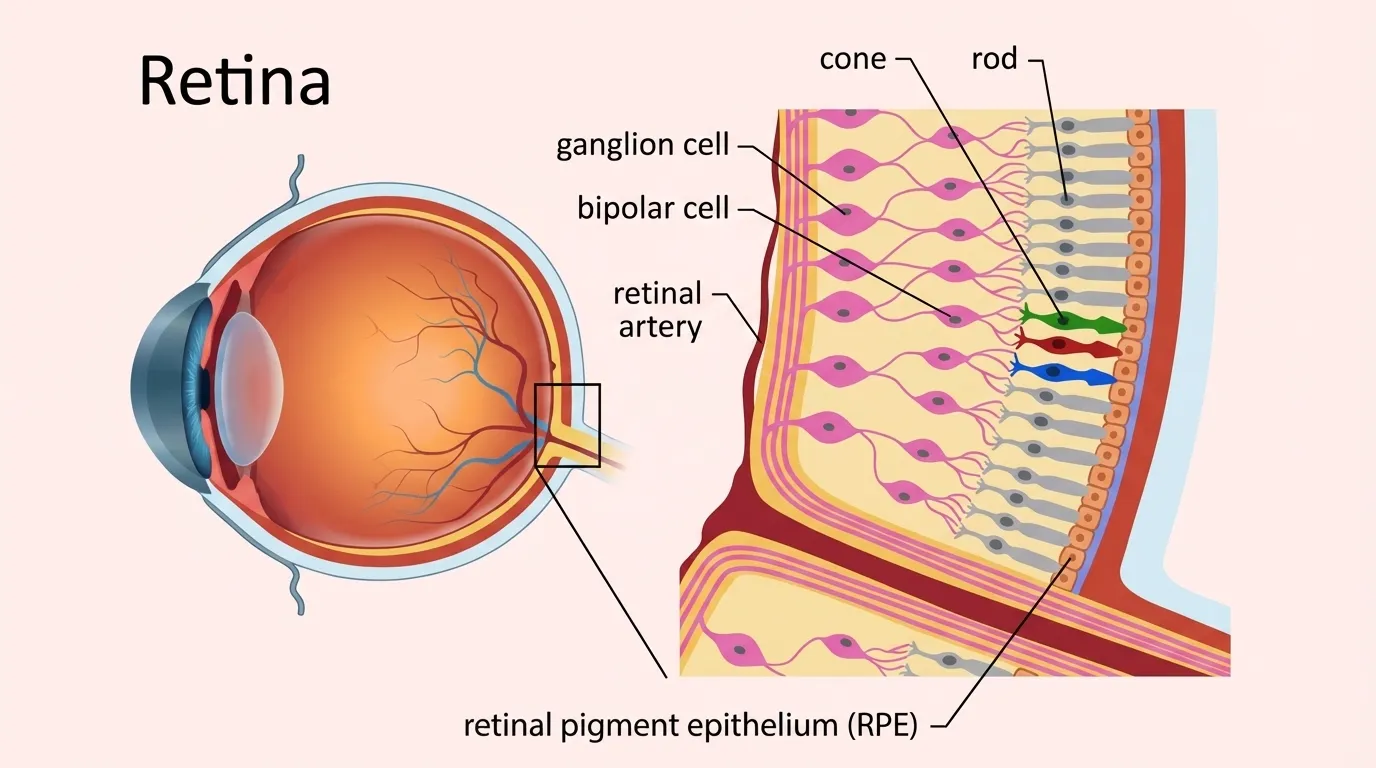
The retina is divided into two main regions. The central retina contains the macula, approximately 5 millimetres in diameter, responsible for sharp, detailed central vision. Within the macula lies the fovea, which provides the sharpest vision. The peripheral retina handles peripheral vision and night vision.
The retina consists of ten distinct layers. The retinal pigment epithelium (RPE) nourishes photoreceptors. The photoreceptor layer contains rods for night vision and cones for color and detailed vision. Other layers contain ganglion cells that process visual signals. Beneath the retina lies the choroid, which supplies oxygen and nutrients.
How the Retina Functions
The retina converts light energy into neural signals through phototransduction. Rod photoreceptors function in low-light conditions, providing black-and-white vision and detecting motion. Approximately 120 million rods are distributed throughout the retina. Cone photoreceptors, numbering 6 to 7 million, are concentrated in the macula and provide color vision and fine detail in bright light.
The retina processes visual information before sending signals to the brain. Bipolar cells transmit signals from photoreceptors to ganglion cells, whose axons form the optic nerve, allowing the retina to enhance contrast and detect edges.
Common Retinal Conditions
Diabetic Retinopathy
Diabetic retinopathy occurs when high blood sugar levels damage retinal blood vessels. It is a leading cause of vision impairment among working-age adults.
The condition develops when elevated blood glucose causes changes to retinal blood vessels. Damaged vessels develop microaneurysms that leak blood and fluid, causing swelling. In advanced stages, oxygen deprivation triggers neovascularization-abnormal blood vessel growth that can rupture and bleed into the vitreous gel.
Non-proliferative diabetic retinopathy (NPDR) is the earliest stage with microaneurysms and small hemorrhages. Proliferative diabetic retinopathy (PDR) is advanced, with abnormal vessels causing bleeding, scarring, and potentially retinal detachment. Severe cases may lead to neovascular glaucoma.
Diabetic macular edema (DME) occurs when fluid leaks into the macula, causing swelling and blurred central vision.
Risk factors include poor blood sugar control, diabetes duration, high blood pressure, high cholesterol, smoking, and kidney disease. Early stages show no symptoms. Progressive symptoms include blurred vision, floaters, dark areas, distorted vision, and vision loss.
Age-Related Macular Degeneration
Age-related macular degeneration (AMD) affects the macula and is a common cause of severe vision loss in people over 60. Central vision is affected while peripheral vision remains intact.
Dry AMD accounts for 85 to 90 percent of cases. It features drusen deposits beneath the retina and gradual photoreceptor loss. Dry AMD progresses slowly, though 10 to 15 percent of cases advance to wet AMD.
Wet AMD involves choroidal neovascularization-abnormal blood vessels growing from the choroid beneath the retina. These vessels leak fluid and blood, causing rapid vision loss. Without treatment, significant vision loss can occur within two years.
Risk factors include age over 60, family history, Caucasian ethnicity, and smoking. Early stages show no symptoms.
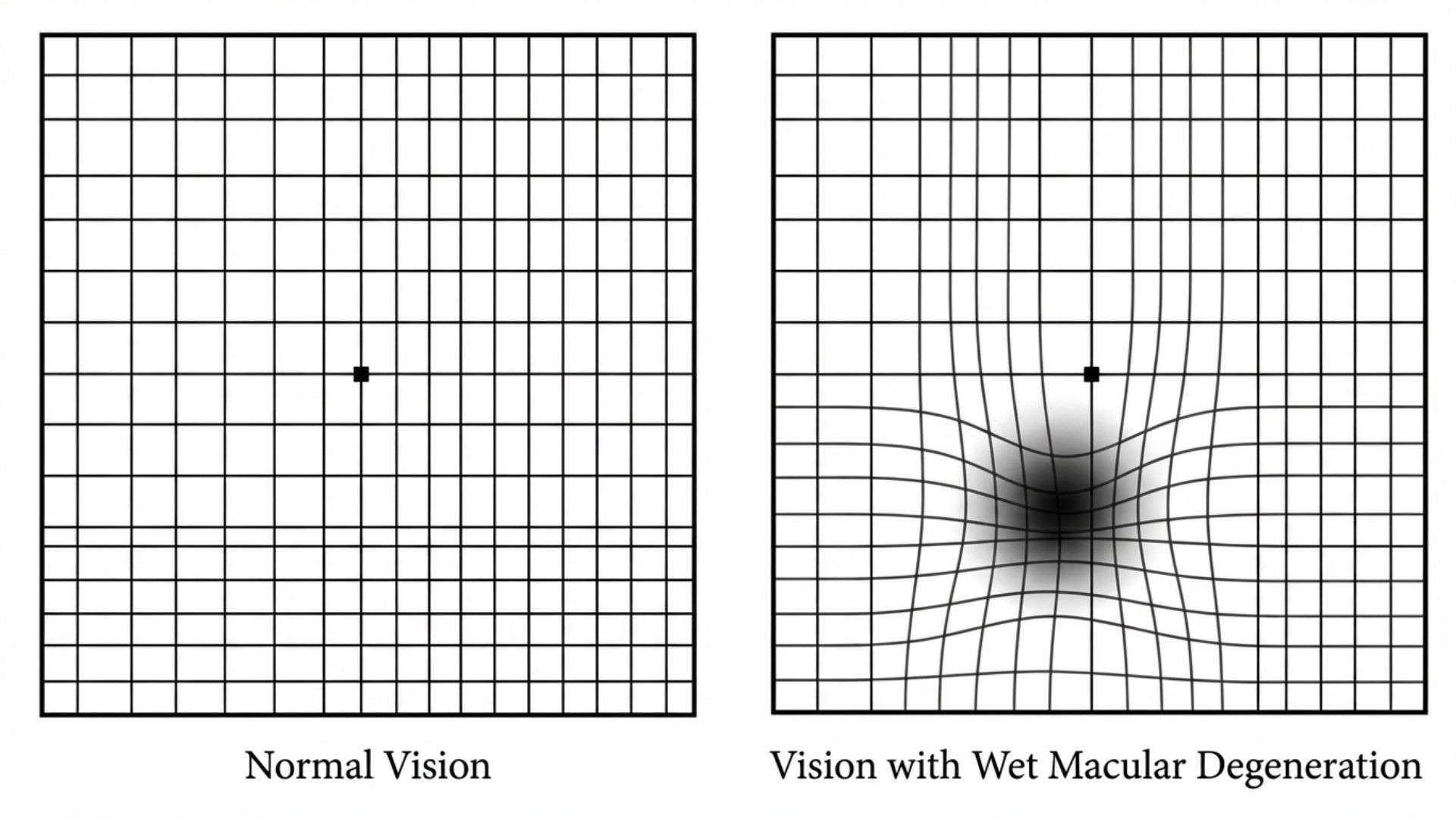
Progressive symptoms include blurred central vision, distortion (monitored with Amsler grid), wavy lines, and dark spots in central vision.
Retinal Detachment
Retinal detachment occurs when the retina separates from underlying tissue, causing vision loss. This is a medical emergency requiring prompt treatment.
Rhegmatogenous detachment occurs when tears allow fluid to seep underneath the retina. Tractional retinal detachment happens when scar tissue pulls the retina away. Risk factors include extreme myopia, previous eye surgery, eye injury, and family history. Symptoms include sudden floaters, light flashes, shadow across vision, and sudden blurring requiring immediate evaluation.
Other Retinal Conditions
Retinal vein occlusion occurs when a vein that carries blood away from the retina becomes blocked, usually by a blood clot. This blockage can cause bleeding, fluid leakage, and swelling in the retina, leading to vision loss. A macular hole is a small break in the macula that can cause blurred or distorted central vision. Epiretinal membrane occurs when scar tissue forms on the retina's surface, causing distorted vision.
Diagnostic Procedures for Retinal Conditions
Accurate diagnosis of retinal conditions requires comprehensive examination by qualified eye care professionals. Our comprehensive eye examination services utilize advanced diagnostic technology to assess retinal health and function.
Dilated Eye Examination
A dilated eye exam is essential for thorough retinal evaluation. Eye drops temporarily enlarge pupils, allowing clear visualization of the entire retina, macula, blood vessels, and optic nerve. This examination detects early changes before symptoms develop.
Optical Coherence Tomography and Fluorescein Angiography
Optical coherence tomography (OCT) provides detailed cross-sectional images of retinal layers using light waves. It detects macular edema, holes, and drusen, measuring retinal thickness with precision.
Fluorescein angiography examines retinal blood flow using fluorescent dye injected into your arm. A camera captures images revealing abnormal vessel growth, leakage, or blockage, valuable for diagnosing diabetic retinopathy, AMD, and vascular conditions.
Fundus Photography and Visual Field Testing
Fundus photography captures detailed color photographs of the retina, optic disc, and blood vessels, providing permanent records for monitoring disease progression.
Visual field testing maps your complete vision field to detect blind spots or decreased sensitivity, helping assess damage from retinal detachment or other conditions affecting peripheral vision.
Amsler Grid Test and Additional Tests
The Amsler grid test screens for central vision changes. Wavy or distorted lines may indicate macular problems.
Electroretinography (ERG) measures the electrical response of the retina's photoreceptors to light stimulation, useful for diagnosing inherited retinal disorders. Indocyanine green angiography reveals blood flow in the choroid layer beneath the retina.
Treatment Procedures for Retinal Conditions
Treatment approaches for retinal conditions vary depending on the specific diagnosis, severity, and individual patient factors. All retinal treatments carry risks that should be carefully discussed with your ophthalmologist before proceeding.
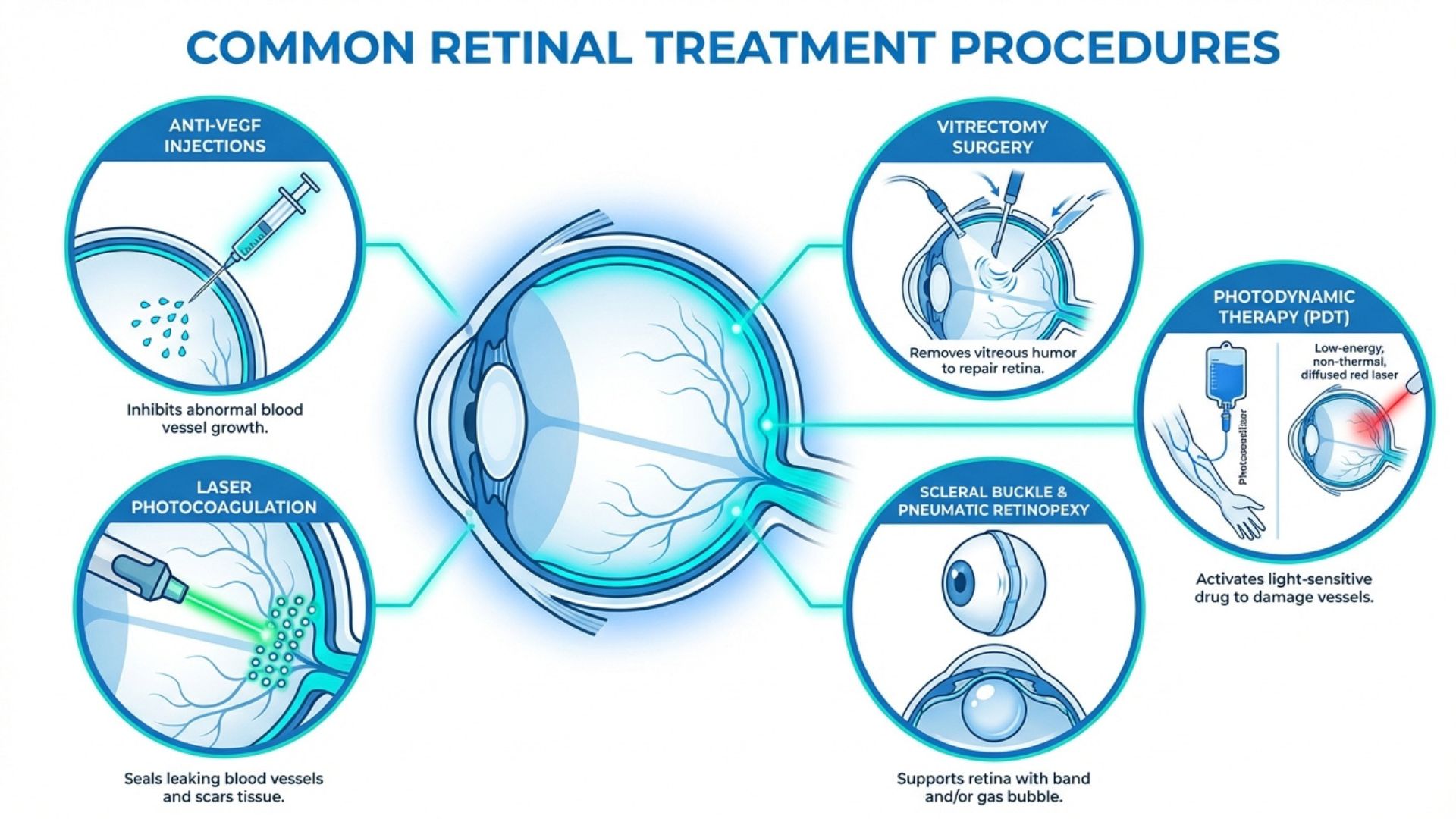
Anti-VEGF Injections
Anti-VEGF injections treat wet AMD, diabetic macular edema, and retinal vein occlusion. These medications block VEGF protein that promotes abnormal blood vessel growth and leakage. The procedure involves injecting medication into the vitreous cavity. Common medications include bevacizumab, ranibizumab, and aflibercept, typically requiring multiple injections over time.
Risks: Eye infection (endophthalmitis), increased eye pressure, retinal detachment, bleeding, cataract progression, inflammation, discomfort, and rarely vision loss. Temporary floaters or light sensitivity may occur.
Laser Photocoagulation
Laser photocoagulation uses focused light to seal leaking vessels or destroy abnormal tissue. Focal laser targets specific leaking vessels in diabetic macular edema. Panretinal photocoagulation (PRP) treats proliferative diabetic retinopathy with hundreds of small burns in peripheral retina, causing abnormal vessels to shrink. Barrier laser treats retinal tears by creating burns that seal the retina to underlying tissue.
Risks: Reduced night vision, decreased peripheral vision, reduced color perception, risk of new tears or detachment, and vision loss in treated areas.
Vitrectomy Surgery
Vitrectomy removes vitreous gel to treat retinal detachment, severe diabetic retinopathy with bleeding, macular hole, and epiretinal membrane. The surgeon makes small incisions, removes vitreous gel, addresses retinal problems, and may inject gas, air, or silicone oil to hold the retina in position. Specific head positioning may be required during recovery.
Risks: Infection, bleeding, retinal detachment, cataract formation, increased eye pressure, inflammation, new retinal tears, double vision, and rarely significant vision loss. Additional surgery may be needed.
Photodynamic Therapy
Photodynamic therapy (PDT) was previously used more commonly for wet AMD but has largely been replaced by anti-VEGF injections as first-line treatment. PDT involves injecting a light-sensitive drug called verteporfin into a vein in your arm. The drug travels through your bloodstream and is absorbed by abnormal blood vessels in the eye. A special low-power laser is then directed at these vessels, activating the drug and causing the abnormal vessels to close.
Risks of Photodynamic Therapy: PDT carries risks including temporary vision changes, light sensitivity requiring sun protection for several days, risk of vision loss, potential damage to surrounding healthy retinal tissue, and possibility that abnormal vessels may reopen requiring repeat treatment.
Pneumatic Retinopexy and Scleral Buckle
Pneumatic retinopexy involves injecting a gas bubble into the vitreous cavity that presses against the detached retina. Scleral buckle surgery uses a flexible band sewn around the eye to push the eye wall toward the retinal tear. Both procedures carry risks including infection, vision changes, and potential need for additional surgery.
Preventive Care and Maintaining Retinal Health
While some retinal conditions result from aging or genetics, several lifestyle measures can help protect retinal health and reduce the risk of vision loss.
Blood Sugar Control for Diabetics
If you have diabetes, maintaining stable blood glucose levels is the single most important factor in preventing diabetic retinopathy or slowing its progression. Work closely with your healthcare team to monitor your blood sugar, take medications as prescribed, and make dietary and lifestyle adjustments to keep glucose levels within target ranges. Even modest improvements in blood sugar control can significantly reduce the risk of retinal complications.
Regular monitoring of hemoglobin A1c levels, which reflect average blood glucose over the previous three months, helps assess long-term glucose control. Most adults with diabetes should aim for an A1c below 7 percent, though individual targets may vary based on other health factors.
Blood Pressure and Cardiovascular Health
High blood pressure damages blood vessels throughout the body, including those in the retina. Managing hypertension through medication, diet, exercise, and stress reduction helps protect retinal blood vessels and reduces risk of retinal vein occlusion and progression of diabetic retinopathy. Similarly, managing cholesterol levels and maintaining cardiovascular health supports retinal vascular health.
Smoking Cessation
Smoking significantly increases the risk of AMD and accelerates its progression. It also contributes to diabetic retinopathy progression. If you smoke, quitting is one of the most beneficial actions you can take for your eye health and overall health. Avoid exposure to secondhand smoke as well, as it also contributes to retinal damage.
UV Protection
While UV radiation's effects on the retina are less direct than on other eye structures, protecting your eyes from excessive sun exposure may contribute to overall eye health. Wear sunglasses that block 100 percent of UVA and UVB radiation when outdoors, and consider wearing a wide-brimmed hat for additional protection.
Nutrition for Eye Health
A diet rich in nutrients that support retinal health may help reduce the risk of AMD and other retinal conditions. Leafy green vegetables contain lutein and zeaxanthin, antioxidants that may protect against AMD. Foods rich in omega-3 fatty acids, such as fatty fish, may also support retinal health. For people with intermediate or advanced dry AMD, the AREDS2 formula supplement may reduce progression risk after consulting with your ophthalmologist.
Eye Protection from Injury
Protect your eyes from injury during activities that pose risk to your eyes. Wear appropriate protective eyewear during sports, when using power tools, when working with chemicals, and in any environment where flying debris or particles may be present. Eye injuries can cause immediate retinal damage or increase the risk of retinal detachment later.
Regular Eye Examinations
Regular comprehensive eye examinations are essential for detecting retinal conditions before symptoms develop or before they progress to advanced stages. Adults with diabetes should have dilated eye examinations at least annually, or more frequently if diabetic retinopathy is detected. Adults over 60 should have comprehensive eye exams every one to two years even without symptoms, as the risk of AMD and other retinal conditions increases with age.
People with high myopia, previous eye surgery, family history of retinal conditions, or other risk factors should discuss appropriate screening schedules with their ophthalmology specialists. Early detection allows for timely intervention that can preserve vision and prevent irreversible damage.
Awareness of Warning Symptoms
Familiarize yourself with symptoms that may indicate retinal problems requiring immediate attention. Seek urgent evaluation if you experience sudden appearance of numerous floaters, sudden flashes of light, shadow or curtain effect across your vision, sudden vision loss, or sudden onset of distortion where straight lines appear wavy. These symptoms may indicate retinal tear, detachment, or other conditions requiring prompt treatment to prevent permanent vision loss.
When to Seek Professional Care
Schedule a comprehensive eye examination with our ophthalmology specialists if you experience sudden changes in vision, new floaters or flashes of light, blurred or distorted central vision, difficulty reading or recognizing faces, progressive loss of peripheral vision, a shadow or curtain effect in your visual field, or any other concerning changes in your vision.
If you have diabetes, maintain regular eye examination schedules even if your vision seems normal, as diabetic retinopathy can progress without symptoms. Similarly, if you have a family history of retinal conditions or other risk factors, discuss appropriate monitoring with your eye care professional.
For sudden onset of symptoms such as significant floater increase, light flashes, or vision loss, seek immediate evaluation as these may indicate conditions requiring urgent treatment.
Conclusion
The retina is a sophisticated tissue that converts light into the neural signals your brain interprets as vision. Understanding retinal anatomy, function, and common conditions affecting the retina is important for maintaining eye health throughout life. While some retinal conditions are age-related or genetic, many can be prevented or their progression slowed through proper management of systemic health conditions, protective lifestyle measures, and regular eye examinations. Various diagnostic and treatment options are available for retinal conditions, though all treatments carry risks that should be carefully considered and discussed with a qualified ophthalmologist.
Important Medical Notice: This information is for general educational purposes and does not replace professional medical advice. Retinal conditions vary in severity and treatment requirements. For personalized assessment and treatment recommendations, please schedule a consultation with our eye care specialists. All surgical procedures and treatments carry risks including infection, bleeding, vision loss, retinal detachment, increased eye pressure, inflammation, cataract development, and in rare cases permanent vision loss.
When to Seek Professional Care
Light-sensitive tissue at the back of the eye processes visual information and transmits signals to the brain, with damage potentially causing significant vision impairment requiring specialist evaluation and treatment.
Please visit the doctor if you have any of the following symptoms:
Sudden appearance of numerous floaters or spots
Flashes of light in peripheral vision areas
Shadow or curtain effect across visual field
Blurred or distorted central vision persisting
Difficulty reading text or recognising familiar faces
Regular retinal examinations enable early detection of conditions before permanent damage occurs, allowing timely intervention to preserve vision and maintain long-term eye health.