Vitreous Humor: Understanding Your Eye's Gel-Like Filling
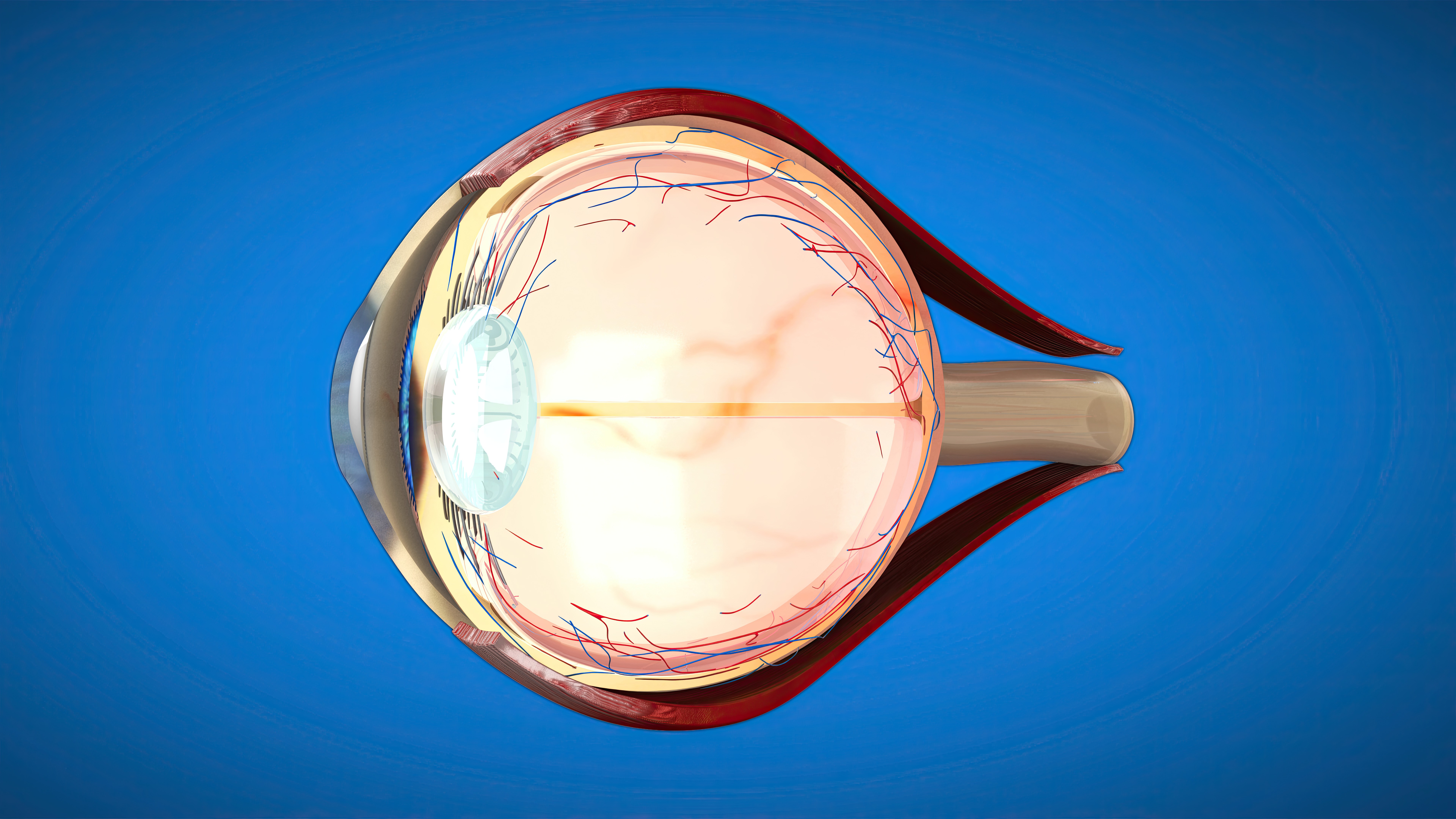
The vitreous humor is a clear, gel-like substance that fills the large space between the lens at the front of your eye and the retina at the back. Making up approximately 80% of your eye's volume, this transparent gel helps maintain your eye's round shape and allows light to pass through to the retina, where visual information is processed. While the vitreous remains stable for much of your life, age-related changes can cause it to liquefy and pull away from the retina, sometimes leading to symptoms like floaters and flashes. Understanding these changes and knowing when to seek professional care is essential for protecting your vision.
Important: All vitreous-related treatments and surgeries carry risks. This information is educational and should not replace individual consultation with a qualified ophthalmologist.
Understanding the Vitreous Humor
The vitreous humor, also called vitreous gel or vitreous body, is a transparent, jelly-like substance occupying the posterior chamber of your eye. Unlike the aqueous humor that flows continuously through the front of the eye, the vitreous is a stable gel that forms during early development and remains relatively unchanged until age-related degeneration begins.
Composed of approximately 98-99% water, the vitreous also contains collagen fibers, hyaluronic acid, proteins, salts, sugars, and specialized cells called phagocytes that help keep the eye clean. This unique composition gives the vitreous its gel-like consistency while maintaining transparency that allows light to pass through unobstructed.
The vitreous serves several important functions. Its primary role is structural support, as the gel fills the cavity between the lens and retina, helping maintain the eye's spherical shape and keeping the retina properly positioned against the back wall of the eye. Additionally, the vitreous provides a clear optical pathway for light to travel from the lens to the retina without distortion.
The vitreous occupies the vitreous cavity, extending from the posterior surface of the lens to the inner surface of the retina. It attaches most firmly to the retina at several key points: the optic nerve head, the macula (the central area responsible for detailed vision), and the peripheral retina in areas of lattice degeneration or pigmentation.
Common Vitreous-Related Conditions
Posterior Vitreous Detachment
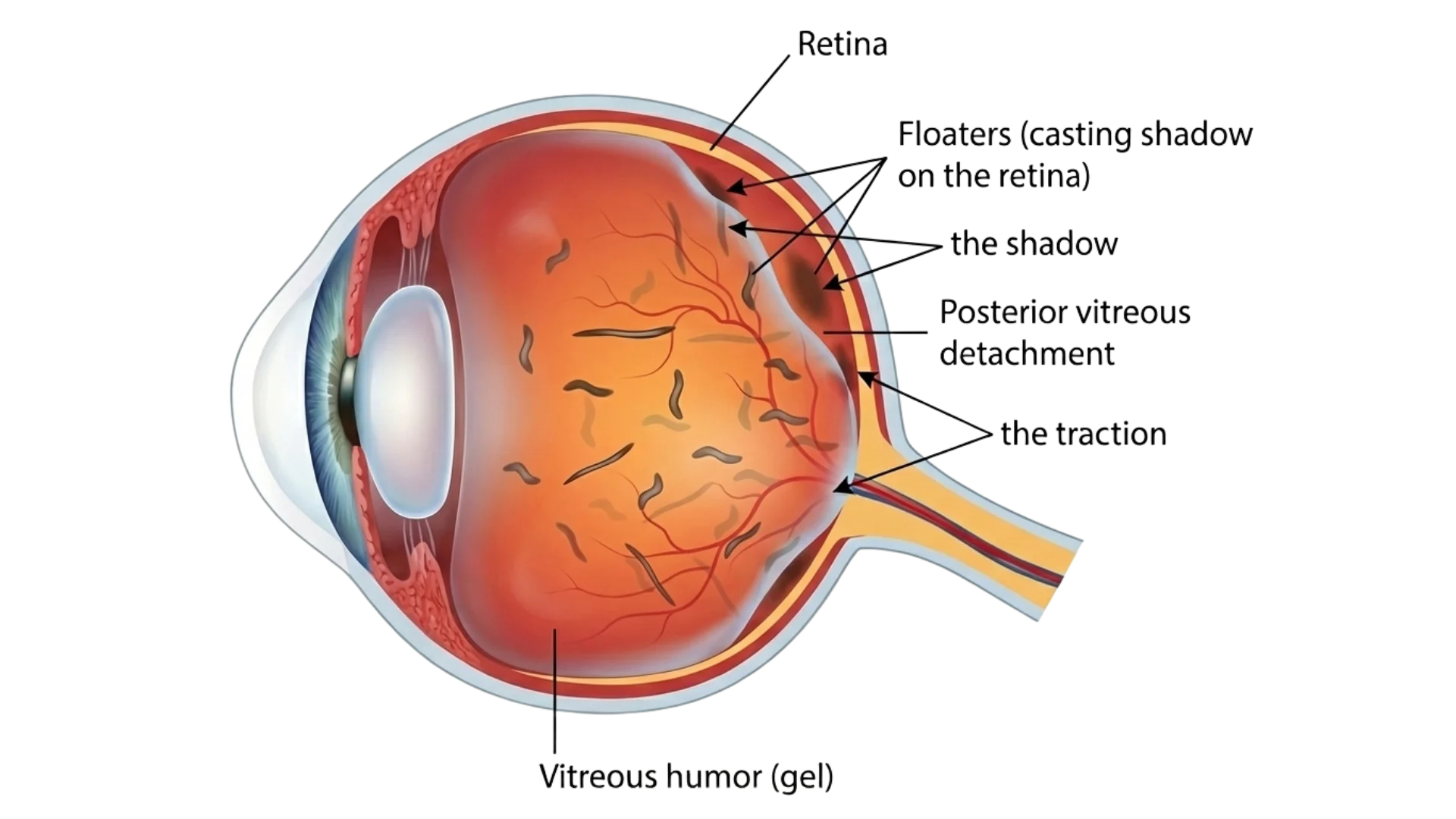
Posterior vitreous detachment (PVD) is a natural age-related process that occurs when the vitreous gel liquefies and separates from the retina. This condition affects most people over age 60 and is more common in individuals who are short-sighted, have undergone cataract surgery, or have experienced eye trauma.
As you age, the collagen fibers within the vitreous break down and the gel gradually liquefies. As liquefaction progresses, the vitreous can no longer maintain its attachment to the retina and begins to collapse forward, pulling away from the retinal surface.
During PVD, the tugging action causes flashes of light, typically seen as brief streaks in your peripheral vision. As the vitreous separates, clumps of collagen fibers and cells cast shadows on the retina, which you perceive as floaters. Most cases of PVD are uncomplicated and require no treatment. However, in approximately 10-15% of cases, the vitreous traction can cause a retinal tear or retinal detachment, which are serious vision-threatening complications.
Floaters and Flashes
Floaters are small specks, threads, or cobweb-like shapes that appear to drift through your field of vision. They are caused by microscopic clumps of gel or cells within the vitreous that cast shadows on the retina. When you look at a plain background such as a white wall or clear blue sky, these shadows become more noticeable.
While floaters can be annoying, they are generally harmless. However, a sudden increase in the number of floaters, particularly if accompanied by flashes of light, may indicate a more serious problem such as vitreous hemorrhage or retinal tear.
Flashes appear as brief streaks or arcs of light, typically in your peripheral vision. They result from the vitreous tugging on the retina, mechanically stimulating the photoreceptor cells. While occasional flashes can occur with PVD, persistent or increasing flashes warrant immediate evaluation.
Other causes of floaters include blood in the vitreous from diabetic retinopathy, retinal vein occlusion, or eye trauma, and inflammatory cells from uveitis.
Vitreous Hemorrhage
Vitreous hemorrhage occurs when blood leaks into the vitreous cavity. This can happen when abnormal blood vessels rupture, as in advanced diabetic retinopathy or age-related macular degeneration, or when healthy vessels tear during retinal tears or detachment.
Symptoms depend on the severity of bleeding. Small hemorrhages may appear as a few new floaters, while larger hemorrhages can cause sudden, severe vision loss. Vitreous hemorrhage requires prompt evaluation to identify and treat the underlying cause. Small hemorrhages may clear on their own over weeks to months, though larger hemorrhages often require surgical removal through vitrectomy.
Epiretinal Membrane
An epiretinal membrane (ERM), also called macular pucker, is a thin sheet of fibrous tissue that grows on the surface of the retina, particularly over the macula. They most commonly develop following posterior vitreous detachment when cells migrate to the retinal surface.
As the membrane contracts, it causes wrinkling of the underlying retinal tissue, leading to symptoms including blurred central vision, distorted vision where straight lines appear wavy (metamorphopsia), difficulty reading, and a gray or cloudy area in central vision.
Many epiretinal membranes cause minimal symptoms and require only monitoring. However, when vision distortion significantly interferes with daily activities, surgical removal through vitrectomy may be recommended, which can improve or stabilize vision in approximately 70-80% of patients.
Vitreomacular Traction
Vitreomacular traction (VMT) occurs when the vitreous remains partially attached to the macula during posterior vitreous detachment. Instead of cleanly separating, the vitreous continues pulling on the delicate macular tissue, potentially causing complications.
Symptoms include blurred or distorted central vision and decreased visual acuity. Persistent traction can cause macular holes, macular edema, or epiretinal membrane formation. Treatment depends on severity: mild cases may be monitored, while significant traction may require ocriplasmin injection or vitrectomy surgery.
Diagnostic Procedures for Vitreous Conditions
Dilated Fundus Examination
A thorough dilated eye examination is essential for evaluating the vitreous and retina. Your ophthalmologist will instill dilating drops to enlarge your pupils, allowing complete visualization of the vitreous cavity and retinal surface. Using specialized lenses and indirect ophthalmoscopy, they can identify vitreous changes, detect retinal tears or detachment, and evaluate any bleeding or inflammation.
Optical Coherence Tomography
Optical coherence tomography (OCT) produces high-resolution cross-sectional images of the retina and vitreoretinal interface. This technology is particularly valuable for diagnosing epiretinal membrane, vitreomacular traction, and macular holes. OCT can visualize attachment points between the vitreous and retina and measure retinal thickness changes.
B-Scan Ultrasonography
When the vitreous is cloudy from hemorrhage or inflammation, B-scan ultrasonography uses sound waves to create images of internal eye structures. This is particularly useful for detecting retinal detachment behind vitreous hemorrhage and evaluating the eye after trauma.
Fluorescein Angiography
Fluorescein angiography involves injecting fluorescent dye and taking photographs as it circulates through retinal blood vessels. This test identifies the source of vitreous hemorrhage, detects abnormal blood vessels, and evaluates retinal blood flow.
Treatment and Surgical Procedures
Observation and Conservative Management
Many vitreous conditions, particularly uncomplicated posterior vitreous detachment with floaters, do not require treatment. Most people adapt to floaters over time as the brain learns to ignore them. Wearing sunglasses in bright conditions can reduce awareness of floaters.
However, if you experience a sudden increase in floaters, new flashes of light, a shadow or curtain in your peripheral vision, or sudden vision loss, seek immediate evaluation to rule out retinal tears or detachment.
Laser Photocoagulation
When a retinal tear is detected, laser photocoagulation creates small burns around the tear, forming scar tissue that seals it and prevents fluid from passing through. This office procedure uses local anesthetic drops and typically takes 10-20 minutes.
Risks of Laser Treatment: Laser photocoagulation carries risks including incomplete treatment requiring additional sessions, peripheral vision loss in the treated area, temporary or permanent visual field defects, rare progression to retinal detachment despite treatment, and inflammation following the procedure.
Pneumatic Retinopexy
For certain retinal detachments in the upper retina, pneumatic retinopexy offers a less invasive option. Your surgeon injects a gas bubble into the vitreous cavity that presses against the detached retina, pushing it back into position.
Risks of Pneumatic Retinopexy: This procedure carries risks including failure requiring additional surgery in 20-30% of cases, development of new retinal tears, cataract formation, increased eye pressure, infection, and potential vision loss.
Following the procedure, you must maintain strict head positioning for several days to keep the gas bubble pressing against the detached area. The gas bubble gradually dissolves over 2-8 weeks. During this period, you cannot fly or travel to high altitudes as pressure changes can cause dangerous bubble expansion.
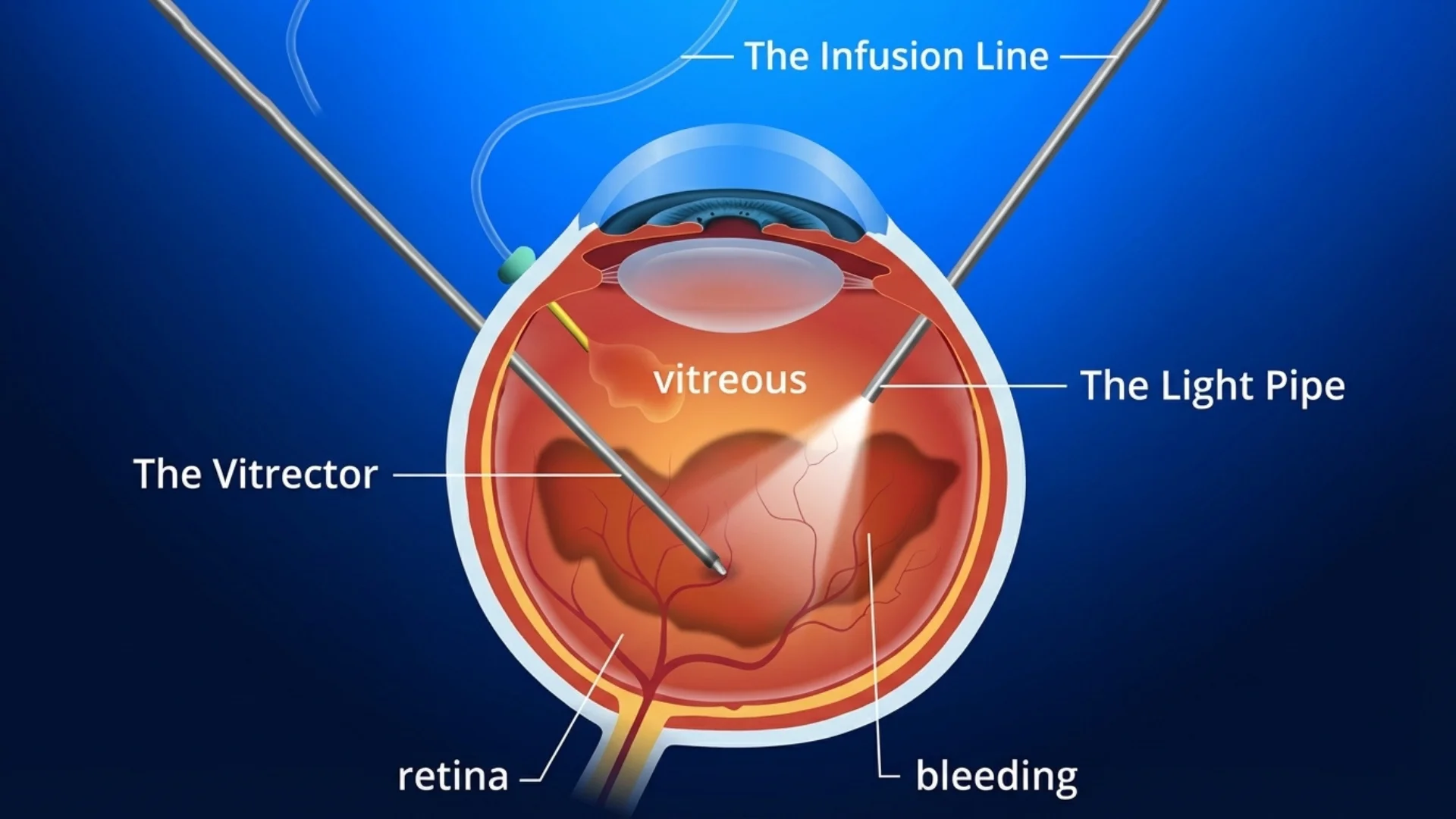
Vitrectomy Surgery
Vitrectomy is a surgical procedure that removes the vitreous gel from your eye. This operation is performed for persistent vitreous hemorrhage, retinal detachment, epiretinal membrane causing significant vision impairment, vitreomacular traction, and severe eye trauma.
Risks of Vitrectomy: All surgical procedures carry risks including infection (endophthalmitis) in approximately 1 in 2,000 cases, retinal detachment in 1-2% of patients, increased eye pressure, cataract formation in nearly all patients over 50 within 1-2 years, bleeding, no improvement or worsening of vision, recurrence of the original condition, and in extremely rare cases loss of the eye. Complications can lead to permanent vision loss or blindness.
Modern vitrectomy is performed through three tiny incisions less than 1 millimetre in size. Your surgeon uses specialized instruments including a light source, vitreous cutter, and other instruments for membrane peeling, laser application, or fluid-air exchange. After removing the vitreous, your surgeon addresses the specific problem and may fill the vitreous cavity with sterile saline, a gas bubble, or silicone oil.
The surgery typically takes 1-3 hours. Most procedures are performed under local anesthesia with sedation. You will go home the same day with specific instructions for positioning and care.
Recovery varies depending on whether gas or oil was used. If a gas bubble was placed, you must maintain specific head positioning for 1-2 weeks and cannot fly until the gas completely dissipates (2-8 weeks). Vision improvement is gradual and may take several months.
Cryotherapy
Cryotherapy uses extreme cold to create adhesions between the retina and underlying tissue. This technique is often used to treat retinal tears or support the retina during surgery. A freezing probe applied to the outside of the eye creates an ice ball that extends through the eye wall to the retina, producing a strong scar bond over 1-2 weeks.
Preventive Care and Vitreous Health Maintenance
Regular Eye Examinations
Routine comprehensive eye examinations allow early detection of vitreous changes and retinal problems. Adults should have dilated eye exams every 1-2 years, or annually if over age 60 or at higher risk due to high myopia, previous eye surgery, or family history of retinal problems.
Managing Systemic Health Conditions
Conditions such as diabetes mellitus and hypertension can affect the vitreous and retina. Poorly controlled diabetes leads to diabetic retinopathy, which can cause vitreous hemorrhage. High blood pressure damages retinal blood vessels and increases the risk of retinal vein occlusion. Maintaining stable blood sugar and blood pressure significantly reduces these risks.
Eye Protection
Trauma is a preventable cause of vitreous problems. Wear appropriate protective eyewear during activities with risk of eye injury such as sports (especially racquet sports, basketball, and baseball), home repair and yard work, industrial work, and when using power tools or chemicals.
Recognizing Warning Signs
Seek urgent evaluation if you experience sudden increase in floaters, new onset of flashes of light, a shadow or curtain obscuring your vision, sudden decrease in vision, or shower of small dots in your vision. These symptoms may indicate retinal tears or detachment, vitreous hemorrhage, or other serious conditions requiring immediate intervention.
When to Seek Professional Care
Schedule a comprehensive eye examination with our ophthalmology specialists if you experience any new floaters or flashes of light, sudden increase in existing floaters, shadow or curtain in your vision, decrease in vision, distorted vision where straight lines appear wavy, or difficulty reading.
For medical emergencies involving sudden severe vision loss, eye pain, or trauma to the eye, contact emergency services immediately.
Conclusion
The vitreous humor plays an essential structural and optical role in your eye, maintaining eye shape and providing a clear pathway for light to reach the retina. While age-related changes to the vitreous are normal, understanding symptoms that may indicate serious complications is important for protecting your vision. Various diagnostic techniques and treatment options, including laser therapy and vitrectomy surgery, are available when complications occur.
Important Medical Notice: This information is for general educational purposes and does not replace professional medical advice. Vitreous conditions vary in severity and treatment requirements. For personalized assessment and treatment recommendations, please schedule a consultation with our eye care specialists. All surgical procedures carry risks including infection, bleeding, vision loss, retinal detachment, cataract formation, increased eye pressure, inflammation, and in rare cases permanent blindness or loss of the eye. All risks, benefits, and limitations should be thoroughly discussed with a qualified ophthalmologist before proceeding with any treatment.
Licensed Healthcare Service: For questions about our services or to book an appointment, please visit our contact page or call our clinic during operating hours. For medical emergencies, please contact emergency services immediately.
When to Seek Professional Care
This transparent gel filling maintains your eye's structure and enables light transmission, though age-related changes may cause it to separate from the retina, sometimes requiring professional intervention.
Please visit the doctor if you have any of the following symptoms:
Sudden shower of new floaters or spots
Flashing lights in peripheral vision areas
Dark curtain or shadow blocking vision
Abrupt decrease in visual clarity overall
Straight lines appearing wavy or distorted
Prompt evaluation by an ophthalmologist ensures timely detection of retinal complications, preserves sight through appropriate treatment, and prevents progression of potentially serious vitreous-related conditions.