Intravitreal Anti-VEGF Injections
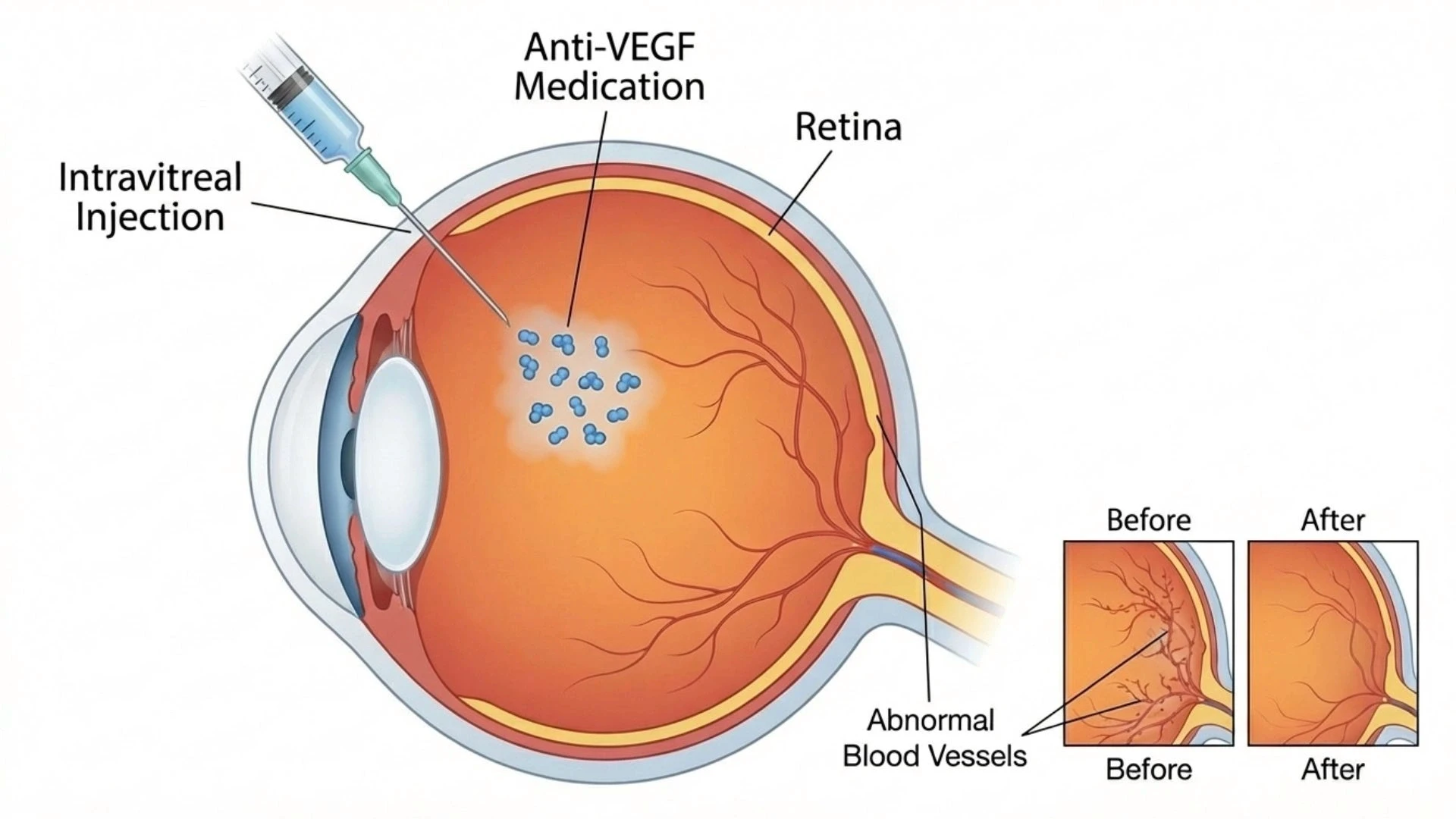
Intravitreal anti-VEGF injections deliver medication directly into the eye to treat conditions caused by abnormal blood vessel growth and leakage. These injections have transformed the management of several sight-threatening retinal conditions, helping to preserve and sometimes improve vision.
Understanding the Treatment
VEGF (vascular endothelial growth factor) is a protein that signals the body to grow new blood vessels. While this is normally beneficial, excessive VEGF in the eye can cause abnormal, fragile blood vessels to develop and existing vessels to leak fluid into the retina.
Anti-VEGF medications block this protein, reducing fluid accumulation and preventing further abnormal vessel growth. The National Eye Institute provides detailed information on how these treatments work for age-related macular degeneration and other conditions.
Conditions Treated
Intravitreal anti-VEGF injections are commonly used for:
Wet age-related macular degeneration (AMD) where abnormal vessels grow beneath the macula
Diabetic macular oedema causing swelling in the central retina
Retinal vein occlusion complicated by macular oedema or abnormal vessel growth
Myopic choroidal neovascularisation in highly short-sighted eyes
Certain other retinal vascular conditions
The Injection Procedure
The procedure is performed in the clinic and typically takes only 10-15 minutes:
Anaesthetic drops thoroughly numb the eye
The eye and surrounding area are cleaned with antiseptic solution to minimise infection risk
The injection is administered through the white of the eye into the vitreous cavity
The injection itself takes only seconds
Most patients report feeling pressure rather than pain. Research from major clinical trials, including CATT and Protocol T studies, has established the effectiveness of these treatments in appropriate patients.
Treatment Schedule
Unlike one-time procedures, anti-VEGF therapy typically requires ongoing treatment:
Initial phase: Monthly injections for the first three to six months
Maintenance phase: Treatment intervals are then adjusted based on your response
Monitoring: Regular examinations including OCT scans assess how your eye is responding
The exact schedule varies depending on the condition being treated, the specific medication used, and individual response. Some patients eventually achieve longer intervals between treatments or may be able to pause therapy.
Potential Risks
While intravitreal injections have a well-established safety profile, patients should be aware of:
Common, usually mild effects:
Temporary redness from small blood vessel breakage on the eye surface
Mild discomfort or foreign body sensation for a day or two
Temporary floaters from small air bubbles
Brief increase in eye pressure
Rare but serious risks:
Eye infection (endophthalmitis) occurs in approximately 1 in 2,000 to 1 in 5,000 injections-strict sterile technique minimises this risk
Retinal detachment is very rare
Damage to the lens causing cataract is uncommon
Your ophthalmologist takes careful precautions to minimise these risks. The benefits of treatment for sight-threatening conditions generally outweigh the small risks involved.
What Results Can Be Expected
Treatment goals and outcomes depend on the condition:
For wet AMD, the primary goal is to prevent further vision loss; some patients experience vision improvement
For diabetic macular oedema, many patients see improvement in vision and reduction in retinal swelling
Response varies between individuals, and some conditions may require long-term or indefinite treatment
Early detection and treatment generally lead to better outcomes, which is why regular eye examinations are important for those at risk.
Medical Disclaimer: This information provides general guidance about intravitreal anti-VEGF injections and should not replace professional medical advice. Treatment outcomes depend on the specific condition, its severity, and individual response to therapy. These injections are one component of managing complex eye conditions that also require ongoing monitoring. Please consult with our ophthalmologists for assessment and a treatment plan tailored to your needs.
Seek immediate attention if you experience: Increasing pain, significant vision decrease, increasing redness, sensitivity to light, or discharge from the eye-these may indicate infection requiring urgent treatment.

