Comprehensive Guide to Paediatric Eye Conditions: Understanding Vision Development, Disorders, and Management
Introduction to Children's Eye Health
Childhood is a period of rapid growth and discovery, and vision plays a pivotal role in how a child interprets the world. It is widely estimated that the vast majority of learning during a child's early years occurs visually. Good vision is not merely about seeing clearly; it is critical for a child's physical coordination, intellectual development, and overall well-being. Unlike adults, children often do not complain about vision problems because they may not realize that their vision is abnormal. They assume everyone sees the world the way they do.
Therefore, vigilance from parents and caregivers is essential. Common signs of concern include frequent rubbing of the eyes, excessive blinking, squinting to see distant objects, tilting the head to one side, or holding reading materials very close to the face. In some cases, a child's eyes may appear to wander or not move in unison. Early detection and intervention are crucial because the visual system is still developing during the first decade of life. If certain conditions are left untreated during this "critical period," they can lead to permanent visual impairment.
This guide explores common and complex paediatric eye conditions, the physiological mechanisms behind them, the diagnostic and surgical procedures available, and the management strategies used to preserve sight in the paediatric population.
The spectrum of paediatric eye disorders ranges from refractive errors, which are easily corrected with glasses, to more complex neurological or structural issues requiring surgical intervention.
1. Refractive Errors and Myopia (Short-sightedness)
Refractive errors occur when the shape of the eye prevents light from focusing directly on the retina. The most prevalent of these in the modern world, particularly in urban environments like Singapore, is Myopia.
The Myopia Epidemic
Myopia is a condition where distant objects appear blurry while near objects remain clear. This occurs because the eyeball grows too long (axial elongation), causing light rays to focus in front of the retina rather than on it.
In Singapore, the prevalence of myopia is among the highest in the world. Statistics suggest that approximately 80% of 18-year-olds in Singapore are myopic. The condition is multifactorial, driven by a combination of:
Genetics: Children with myopic parents are at a higher risk.
Environmental Factors: Lack of outdoor time and excessive near-work (reading, tablets, smartphones) are significant contributors.
Why Myopia Progression Matters: Myopia usually begins in early childhood and progresses until the eye stops growing in early adulthood. High myopia (severe short-sightedness) is not just a prescription issue; it increases the lifelong risk of sight-threatening conditions such as retinal detachment, myopic maculopathy, glaucoma, and early-onset cataracts.
2. Amblyopia (Lazy Eye)
Amblyopia, widely known as "lazy eye," is a neuro-developmental disorder where vision in one (or rarely both) eyes does not develop properly during childhood. It is a leading cause of vision loss in children.
Pathophysiology
In a healthy visual system, the brain receives clear images from both eyes and fuses them into a single 3D image. In amblyopia, the neural pathways between the affected eye and the brain are not properly stimulated. If one eye sends a blurry or conflicting image, the brain may learn to ignore or "suppress" input from that eye to avoid double vision. Over time, the brain favors the stronger eye, and the vision in the weaker eye stops developing.
Causes of Amblyopia:
Strabismic Amblyopia: Caused by misaligned eyes.
Refractive Amblyopia: Caused by a significant difference in prescription between the two eyes (anisometropia) or high prescription in both eyes.
Deprivation Amblyopia: Caused by a physical obstruction that blocks light from entering the eye, such as a droopy eyelid (ptosis) or a childhood cataract. This is the most severe form and requires urgent treatment.
3. Strabismus (Squint / Crossed Eyes)
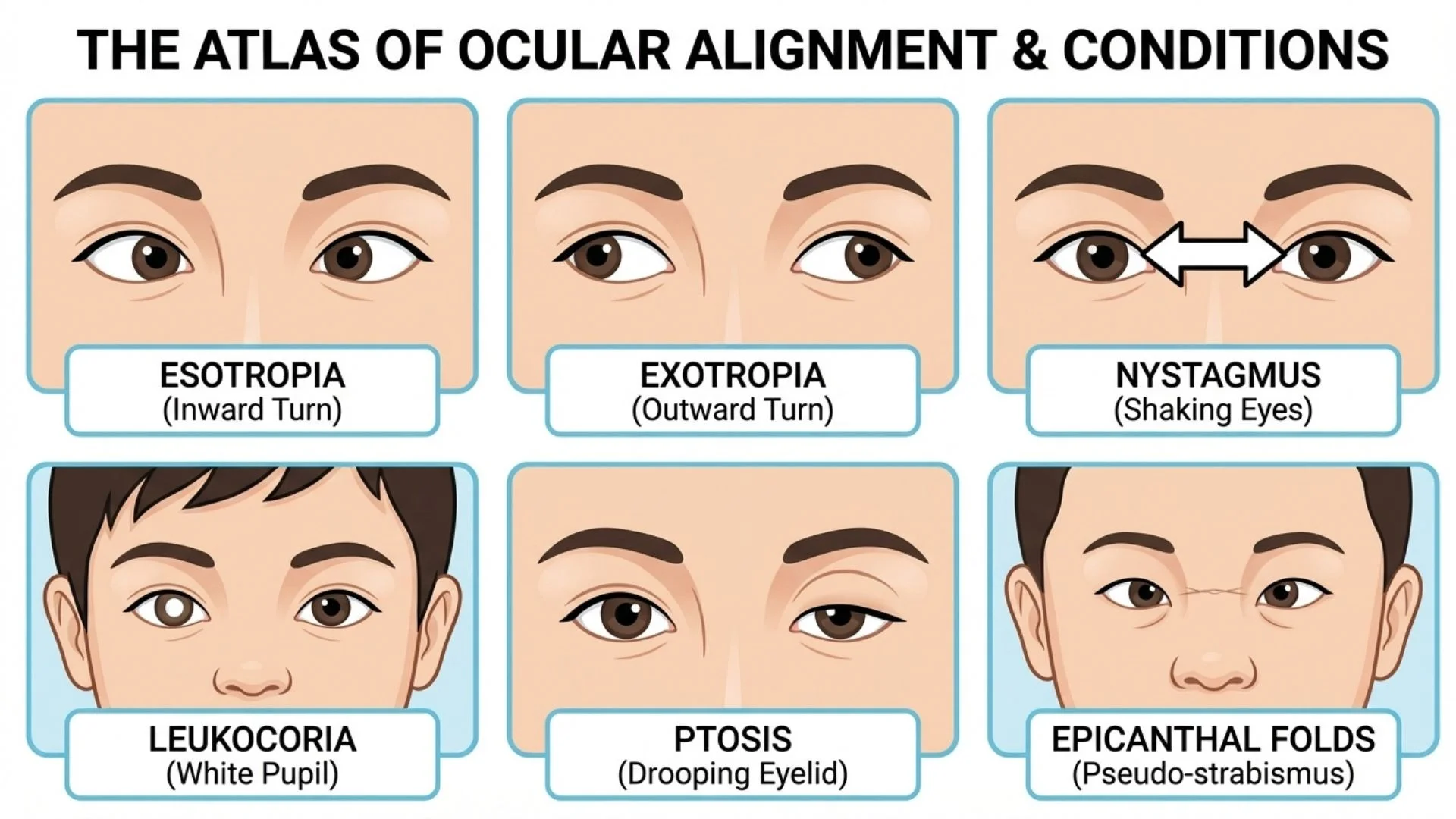
Strabismus is a condition where the eyes do not align properly. One eye may look straight ahead while the other turns inward, outward, upward, or downward. This is caused by an abnormality in the neuromuscular control of eye movement.
Types of Strabismus:
Esotropia: The eye turns inward towards the nose ("crossed eyes").
Infantile Esotropia: Appears within the first 6 months of life.
Accommodative Esotropia: Develops usually between 6 months and 2.5 years, often linked to uncorrected farsightedness (hyperopia).
Exotropia: The eye deviates outward (away from the nose). This is less common than esotropia but frequently seen in intermittent forms when a child is tired or daydreaming.
Strabismus destroys binocular vision and depth perception (stereopsis). If left untreated, it is a primary cause of amblyopia.
4. Structural and Eyelid Abnormalities
Ptosis (Drooping Eyelid)
Ptosis refers to the drooping of the upper eyelid. In children, this is often congenital (present at birth) due to the poor development of the levator muscle responsible for lifting the eyelid. If the lid droops low enough to cover the pupil, it blocks visual input and causes deprivation amblyopia.
Nasolacrimal Duct Obstruction (Blocked Tear Duct)
Many infants are born with a blocked tear duct, causing excessive tearing (epiphora) and discharge. Tears are produced normally but cannot drain into the nose because the membrane at the end of the tear duct has not opened. While many cases resolve spontaneously, persistent obstruction can lead to recurrent infections and requires intervention.
5. Lumps and Bumps: Stye and Chalazion
Eyelids contain oil glands (Meibomian glands) that can become blocked.
Stye (Hordeolum): An acute, painful, red lump near the edge of the eyelid, usually caused by a bacterial infection of a lash follicle.
Chalazion: A painless (or less painful), firm lump caused by a non-infectious blockage and inflammation of an oil gland (lipogranuloma).
6. Serious Pathologies: Cataracts and ROP
Congenital Cataracts
While cataracts are associated with aging, they can occur in newborns. A cataract is an opacification (clouding) of the eye's natural lens. In infants, this blocks light from reaching the retina. Unlike adult cataracts which can be monitored, congenital cataracts are an ocular emergency. Immediate removal is often required to allow the visual pathways to develop; otherwise, permanent profound amblyopia occurs.
Retinopathy of Prematurity (ROP)
Retinopathy of Prematurity is a potentially blinding disease affecting premature babies born before 31 weeks of gestation or with low birth weight. Abnormal blood vessels grow on the retina, which can leak or bleed, leading to scarring and retinal detachment. ROP screening protocols in neonatal intensive care units (NICUs) are vital for timely laser treatment or anti-VEGF injections.
Diagnostic Procedures
1. Cycloplegic Refraction Children have very strong focusing muscles that can mask their true refractive error. To get an accurate measurement, eye care professionals use cycloplegic eye drops. These drops temporarily paralyze the focusing muscle and dilate the pupil. This allows the optometrist or ophthalmologist to determine the full extent of hyperopia (farsightedness), myopia, or astigmatism.
2. Orthoptic Assessment This involves assessing binocular vision and eye movements. Tests include cover-uncover tests to detect strabismus and stereo-acuity tests to measure 3D vision.
Non-Surgical Interventions
1. Amblyopia Therapy (Patching and Penalization) The gold standard for treating lazy eye is forcing the brain to use the weaker eye, as demonstrated by numerous clinical trials.
Occlusion Therapy (Patching): An adhesive patch is worn over the good eye for a specific number of hours daily.
Pharmacological Penalization: Atropine drops are placed in the good eye to blur its vision temporarily, encouraging the use of the amblyopic eye.
Dichoptic Training: Newer therapies involve using digital devices or virtual reality (VR) where different images are presented to each eye, encouraging the brain to combine them.
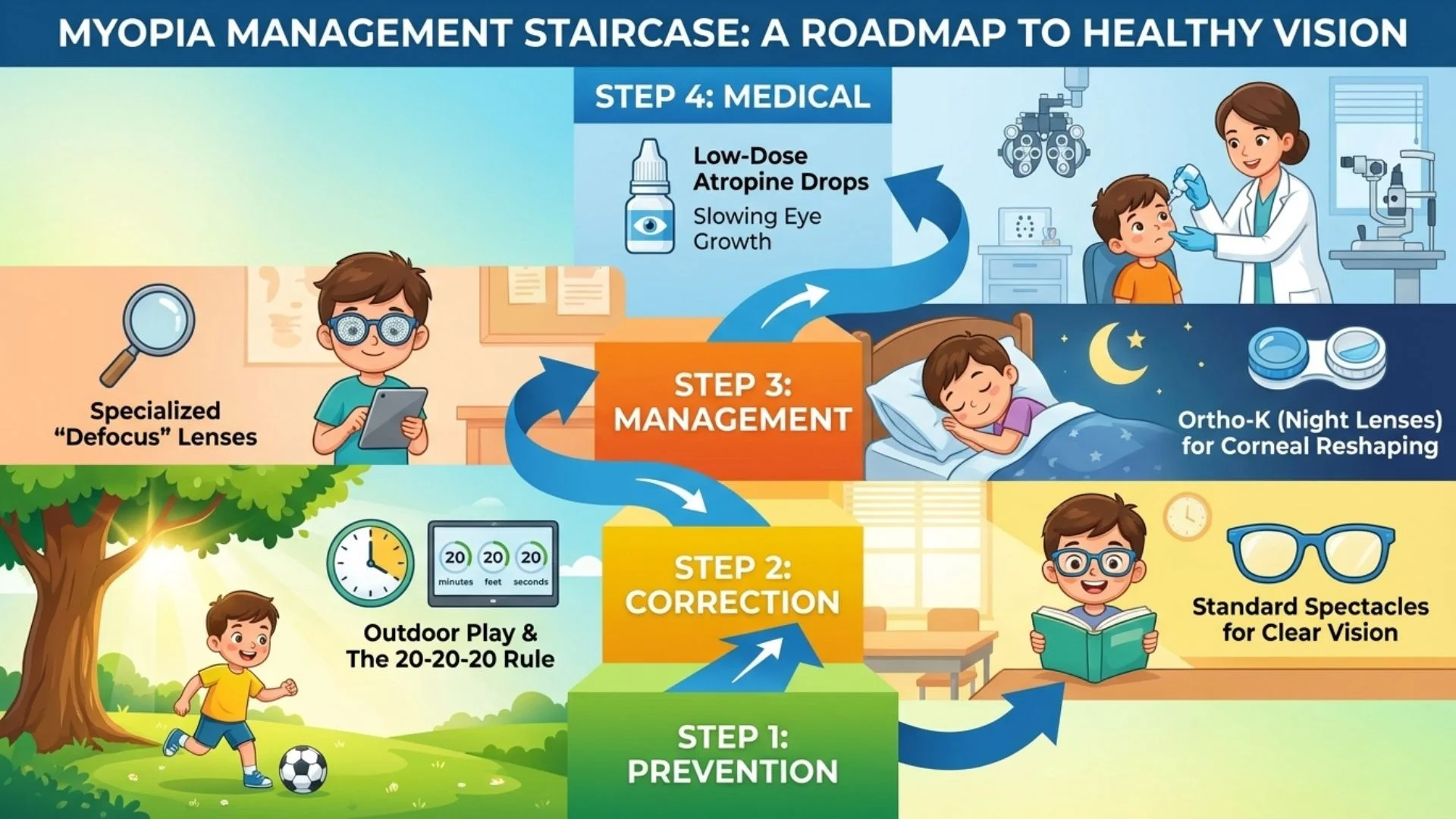
2. Myopia Management Strategies To slow the progression of short-sightedness, several evidence-based methods are utilized:
Low-Dose Atropine Eye Drops: Studies suggest that low concentrations of atropine can slow the elongation of the eyeball without the side effects of full-strength drops.
Specialized Optical Lenses: Spectacles or contact lenses designed with peripheral defocus technology to reduce the stimulus for the eye to grow.
Surgical Procedures
When glasses and therapy are insufficient, or when structural defects are present, surgery becomes necessary.
1. Strabismus Surgery This surgery involves tightening or loosening the eye muscles to align the eyes, with high success rates reported in paediatric populations.
Procedure: The surgeon makes a small incision in the conjunctiva (the clear covering of the eye) to access the extraocular muscles. To weaken a muscle (Recession), it is detached and reattached further back on the eye. To strengthen a muscle (Resection), a section of the muscle is removed to shorten it.
Adjustable Sutures: In some cases, adjustable sutures are used, allowing the surgeon to fine-tune the eye alignment shortly after the surgery while the patient is awake, improving precision.
2. Peadiatric Cataract Extraction Removing a cataract in a child is more complex than in an adult.
Procedure: The cloudy lens is removed (lensectomy). Depending on the child's age, an intraocular lens (IOL) implant may be inserted immediately, or the eye may be left "aphakic" (without a lens) with the vision corrected via contact lenses until the eye grows large enough for an implant.
Posterior Capsulotomy: In young children, the posterior capsule of the lens bag is also opened, and the anterior vitreous is removed (anterior vitrectomy) to prevent the visual axis from becoming cloudy again.
3. Nasolacrimal Duct Probing If a blocked tear duct does not resolve by age one, a probing procedure is performed.
Procedure: A thin, blunt metal wire (probe) is gently passed through the tear duct to break the membranous obstruction. This is usually a quick procedure done under general anesthesia. If probing fails, silicone tube intubation or balloon dacryoplasty may be required.
4. Ptosis Repair Surgery to correct drooping eyelids aims to lift the lid to clear the visual axis and improve symmetry.
Levator Resection: Tightening the levator muscle is the most common method if the muscle has some function.
Frontalis Sling: If the muscle is extremely weak, the eyelid is connected to the frontalis muscle (forehead muscle) using a sling material (synthetic or harvested tissue), allowing the child to lift their eyelid by raising their eyebrows.
While genetic factors play a significant role in paediatric eye conditions, environmental modifications and proactive care are essential for management and prevention.
Lifestyle Modifications for Myopia Control
Research underscores the importance of environmental factors in the onset and progression of myopia.
Outdoor Time: Increased time spent outdoors is protective against the onset of myopia. The high intensity of outdoor light triggers the release of dopamine in the retina, which helps inhibit the elongation of the eyeball. Parents are encouraged to let children spend at least 2 hours a day outdoors.
Visual Hygiene: The "20-20-20 rule" is often recommended: for every 20 minutes of near work (reading or screen time), look at something 20 feet away for at least 20 seconds.
Reading Distance: Ensure children hold books or screens at an appropriate distance (at least 30-40cm away) and ensure the room is well-lit.
Nutritional Interventions
Proper nutrition supports overall ocular health.
Omega-3 Fatty Acids: Research indicates that omega-3 fatty acids (found in fish like salmon and tuna) are essential for retinal development. Some studies suggest they may play a role in slowing myopia progression and managing dry eye symptoms.
Vitamins A, C, and E: These antioxidants support the health of eye tissues. A diet rich in leafy greens, carrots, and colorful fruits provides these essential nutrients.
Hygiene for Eyelid Conditions
For recurrent styes or chalazia (meibomian cysts), eyelid hygiene is the primary remedy.
Warm Compresses: Applying a warm towel to the closed eyelids for 5 to 10 minutes twice a day helps liquefy the oil in blocked glands.
Lid Massage: Gentle massage helps drain the liquefied oils.
Lid Scrubs: Cleaning the eyelid margins with diluted baby shampoo or dedicated lid wipes removes bacteria and debris that clog the glands.
The Role of Regular Screening
Many paediatric eye conditions, such as amblyopia and glaucoma, are asymptomatic in the early stages. Children rarely report vision loss because they adapt to it.
Newborn Screening: Paediatricians check for the "red reflex" at birth to rule out congenital cataracts or retinoblastoma.
Pre-School Screening: Visual acuity and alignment checks should happen before school entry (ages 3 to 5) to catch amblyopia while it is still treatable.
School Screening: Annual checks are vital, especially in myopia-prone regions like Singapore, to ensure refractive errors are corrected promptly.
Understanding the Risks
Parents should be aware that all medical interventions carry risks.
Surgical Risks: While paediatric eye surgeries generally have high success rates, complications can include infection, bleeding, reaction to anesthesia, or the need for re-operation (common in strabismus).
Contact Lens Risks: Children using contact lenses for myopia control or aphakia are at risk of microbial keratitis (corneal infection). Strict hygiene compliance is mandatory.
Amblyopia Therapy Risks: Patching can be emotionally difficult for the child and stressful for the family. In rare cases, excessive patching can induce "reverse amblyopia" in the good eye, though this is usually reversible.
Conclusion
Paediatric ophthalmology is a specialized field dedicated to protecting a child's vision for life. From the high prevalence of myopia in Singapore to the complexities of congenital abnormalities, the range of conditions is vast. However, with modern diagnostic tools, timely surgical interventions, and effective management therapies like atropine and patching, the prognosis for most children is excellent. The key lies in early detection, ensuring that children undergo regular eye examinations so that potential issues are identified and treated during the critical window of visual development.
Important Medical Notice: This information provides general educational content about paediatric eye conditions and refractive errors and should not replace professional medical advice. For personalized assessment and treatment recommendations, please schedule a consultation with our eye care specialists. All vision correction methods including spectacles, contact lenses, and surgical procedures carry risks and limitations. Contact lenses carry risks of infection and corneal complications. Surgical corrections carry risks including infection, vision loss, need for additional procedures, and in rare cases permanent blindness. All options should be thoroughly discussed with a qualified ophthalmologist.
Licensed Healthcare Service: Our clinic operates in accordance with healthcare regulations. For questions about our services or to book an appointment, please visit our contact page or call during operating hours. For medical emergencies, contact emergency services immediately.
When to Seek Professional Care
Children's vision develops rapidly during early years, and undetected eye disorders can lead to permanent visual impairment if left untreated during the critical developmental period. Please visit the doctor if your child has any of the following symptoms:
Frequent eye rubbing or excessive blinking habits
Squinting to see distant objects or boards
Eyes appearing misaligned or wandering independently
Holding books or devices unusually close
Tilting head to one side when viewing
Early screening and timely intervention during childhood ensure proper visual development, preventing lifelong complications and preserving your child's sight and learning abilities.

