Comprehensive Guide to Eyelid Health: Understanding Blepharitis, Chalazia, and Styes
The human eye is often compared to a camera, but without the protective shutter and lens cleaning mechanisms of the eyelids and eyelashes, the delicate structures of the eye would sustain damage almost instantly. The eyelids (palpebrae) and eyelashes are not merely aesthetic features; they form the "adnexa" of the eye: a complex defensive system designed to protect the globe, distribute tears, and sweep away airborne debris.
However, because of their constant exposure to the environment and their complex anatomy involving skin, muscle, mucous membranes, and oil glands, the eyelids are highly susceptible to inflammation and infection. Conditions such as Blepharitis, Chalazia (eyelid cysts), and Styes (hordeolums) are among the most common reasons patients seek ophthalmic care. While often dismissed as minor annoyances, chronic eyelid conditions can lead to debilitating dry eye disease, corneal scarring, and fluctuating vision if left unmanaged.
This guide offers an extensive look into the pathology, symptoms, diagnosis, and medical management of these conditions, helping you understand the importance of lid hygiene and professional care.
The Anatomy of the Eyelid Margin
To understand why eyelids get swollen or infected, one must first understand the anatomy of the eyelid margin: the edge where the skin meets the moist conjunctiva.
The Meibomian Glands
Hidden vertically within the firm tarsal plates of the upper and lower eyelids are the Meibomian glands. There are approximately 25 to 40 glands in the upper lid and 20 to 30 in the lower lid. These specialized sebaceous glands secrete meibum: an oil that forms the outermost layer of the tear film.
Function: This oil layer floats on top of the watery tears, preventing them from evaporating into the air.
Dysfunction: When these glands block, tears evaporate too quickly, leading to "Evaporative Dry Eye."
The Eyelash Follicles
The eyelashes grow in 2 to 3 irregular rows along the anterior margin of the lid. Like all hair follicles, they are associated with glands (Glands of Zeis) and can become a breeding ground for bacteria or microscopic mites if hygiene is poor.
Blepharitis: The Silent Chronic Condition
Blepharitis is the medical term for general inflammation of the eyelids. It is notoriously chronic, meaning that while symptoms can wax and wane, the underlying tendency for inflammation often persists for years. It is frequently associated with systemic skin conditions like Rosacea, Seborrheic Dermatitis (dandruff), or Eczema.
Blepharitis is clinically categorized by its location on the eyelid:
1. Anterior Blepharitis
This inflammation occurs at the front edge of the eyelid, surrounding the base of the eyelashes.
Staphylococcal Blepharitis: Caused by an overgrowth of Staphylococcus bacteria. These bacteria produce exotoxins that irritate the eye surface, leading to redness and potential hypersensitivity reactions in the cornea (marginal keratitis).
Seborrheic Blepharitis: Associated with dandruff of the scalp and brows. It manifests as greasy, waxy scales on the lashes.
2. Posterior Blepharitis (Meibomian Gland Dysfunction)
This is the more common form, affecting the inner edge of the eyelid where the Meibomian glands open.
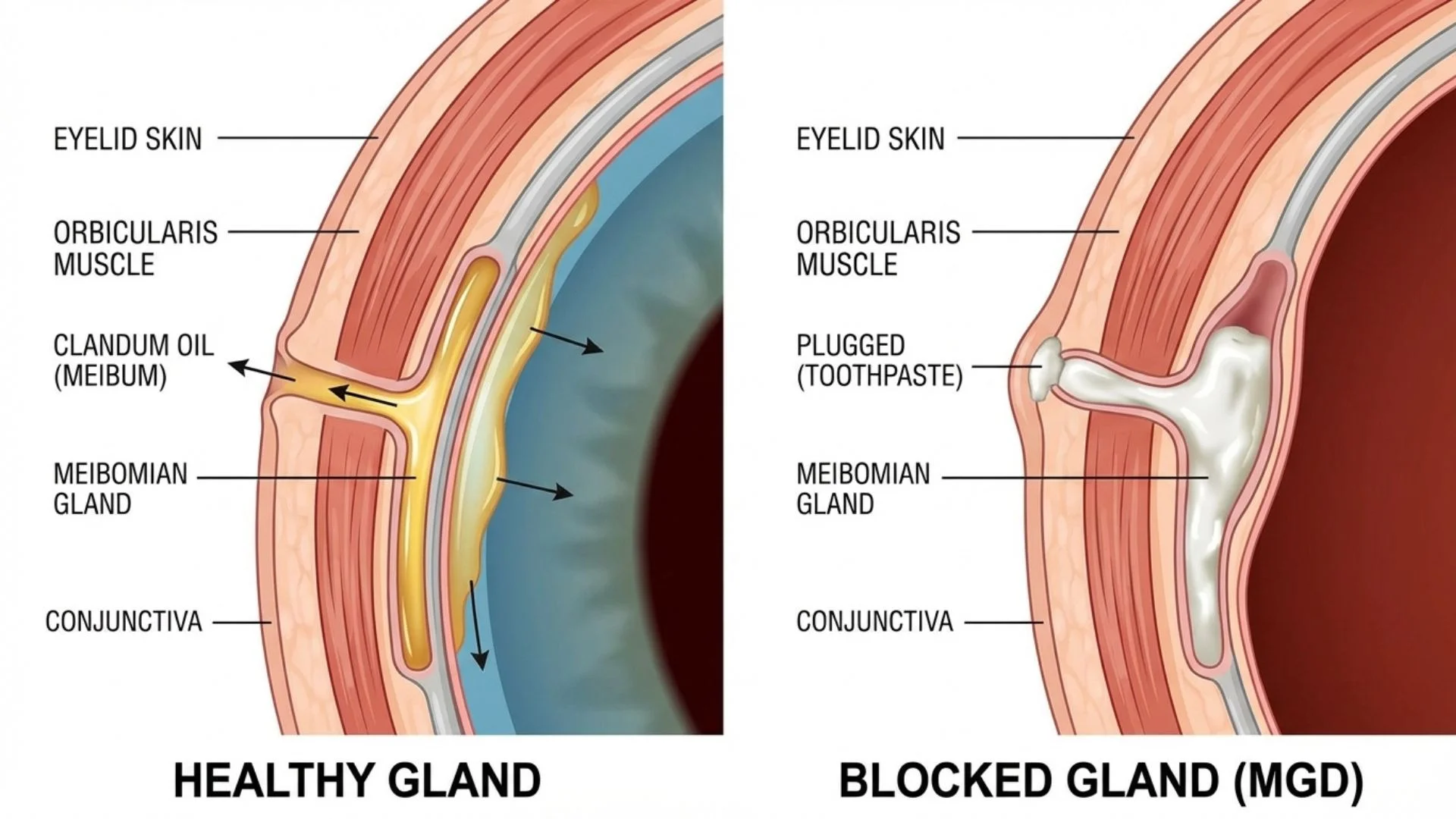
Mechanism: In this condition, the oil secretions become thickened, turning from a clear olive-oil consistency to a cloudy, toothpaste-like texture. This blocks the gland openings (orifices).
Consequence: The blocked glands cannot secrete oil, causing the tear film to become unstable. Over time, chronic blockage can cause the glands to atrophy (die off), which is irreversible.
The Role of Demodex Mites
A significant and often overlooked cause of blepharitis is Demodex infestation. Demodex folliculorum and Demodex brevis are microscopic mites that live in hair follicles and sebaceous glands. While present in small numbers on most adults, an overpopulation can trigger severe inflammation.
Signs: The hallmark sign of Demodex blepharitis is "cylindrical dandruff": waxy cuffs that form around the base of the eyelashes.
Eyelid Lumps: Distinguishing Styes from Chalazia
When the glands or follicles in the eyelid become blocked or infected, localized lumps develop. It is crucial to distinguish between a Stye and a Chalazion, as their treatments differ significantly.
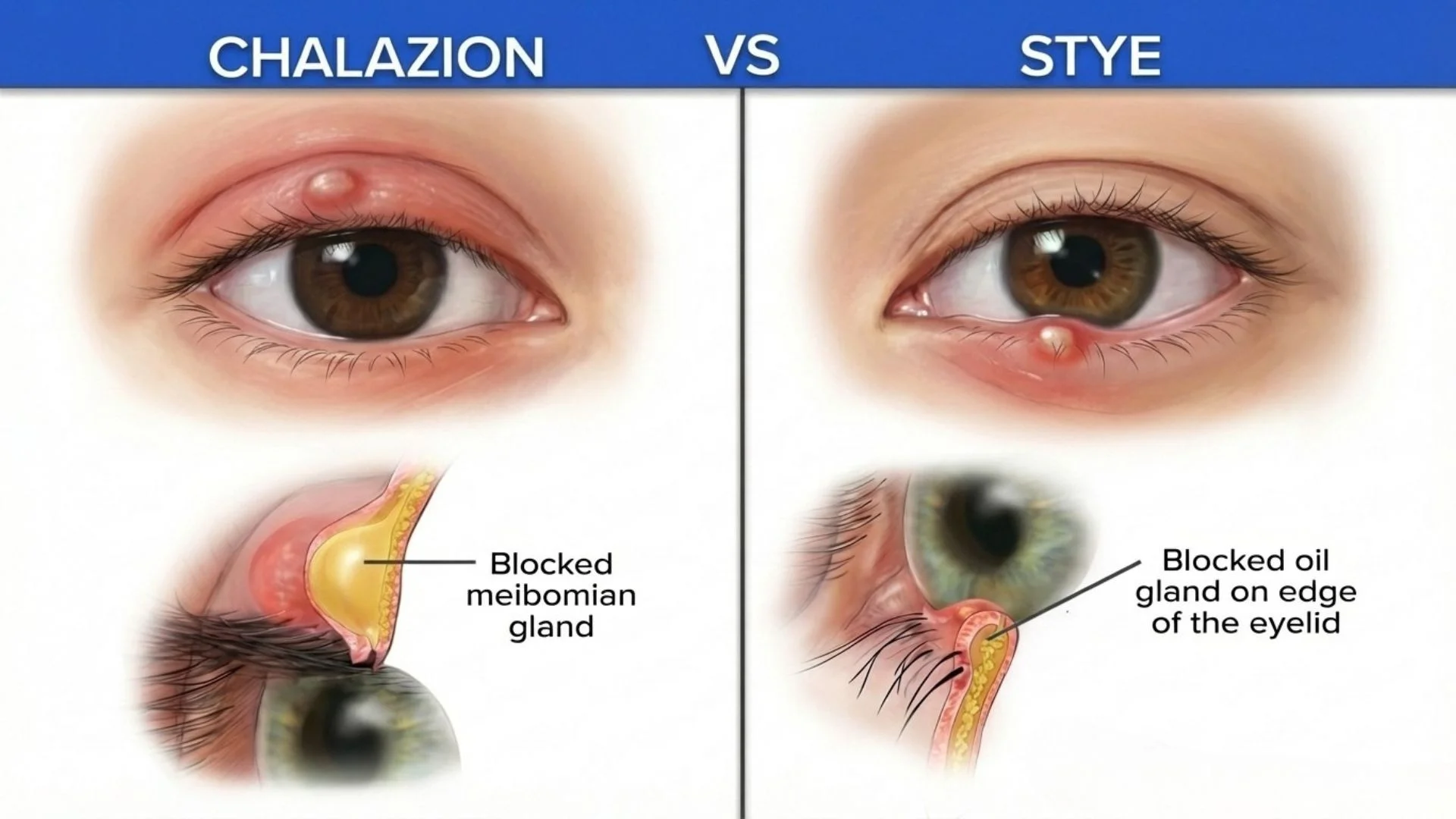
The Stye (Hordeolum)
A stye is an acute, active infection. It is essentially an abscess in the eyelid.
External Hordeolum: An infection of the eyelash follicle or the Gland of Zeis. It appears as a red, painful bump at the very edge of the lid, often looking like a pimple with a yellow head.
Internal Hordeolum: An infection of a Meibomian gland deeper inside the eyelid.
Symptoms: Intense pain, tenderness to touch, redness, heat, and localized swelling.
Cause: Bacterial infection (usually Staph).
The Chalazion (Meibomian Cyst)
A chalazion is a chronic, sterile inflammatory granuloma. It is usually not an infection.
Formation: It occurs when a Meibomian gland becomes obstructed. The gland continues to produce oil, but the oil cannot escape. The gland swells, and eventually, the gland wall may rupture, leaking oil into the surrounding eyelid tissue. The body's immune system perceives this oil as a foreign substance and walls it off with inflammatory cells, creating a hard lump.
Symptoms: Typically painless (or only mildly tender), firm, and slow-growing. It generally points toward the inside of the eyelid.
Visual Impact: A large chalazion can press on the cornea, physically warping its shape and inducing astigmatism, causing blurred vision.
Signs and Symptoms of Lid Disease
Patients with blepharitis or lid lumps often attribute their symptoms to "tired eyes" or "allergies." However, specific clinical signs point to lid disease:
Morning Symptoms: Symptoms are often worse upon waking because the eyelids have been in contact with the ocular surface all night, allowing bacterial toxins and inflammatory mediators to accumulate in the tear film.
Crusting and Matting: Eyelashes may be stuck together with dried discharge ("sleep") in the mornings.
Grittiness: A sensation of sand or a foreign body in the eye.
Red Lid Margins: The rims of the eyes appear pink or bloodshot (Hyperemia).
Photophobia: Increased sensitivity to bright lights or screens.
Fluctuating Vision: Vision that is blurry but clears temporarily after a hard blink. This indicates that the blur is caused by an unstable tear film rather than a refractive error in the eye itself.
Contact Lens Intolerance: Patients may find they can no longer wear their contact lenses comfortably for long periods due to dryness and lipid deposits clouding the lens.
Diagnostic Procedures for Eyelid Conditions
Diagnosing lid disease goes beyond a simple visual inspection. Ophthalmologists use specialized equipment to assess the severity of the gland dysfunction and the health of the ocular surface.
Slit-Lamp Biomicroscopy
The standard examination uses a high-powered microscope. The doctor looks for:
Telangiectasia: Tiny, spider-web blood vessels on the eyelid margin, a hallmark of chronic inflammation and Ocular Rosacea.
Pouting: The openings of the Meibomian glands may look swollen or capped with white keratin.
Lash Debris: Presence of scurf, collarettes, or mites.
Meibomian Gland Expression
The clinician applies mechanical pressure to the eyelid (using a finger, cotton tip, or specialized paddle) to express the meibum.
Healthy: Clear, free-flowing oil.
Grade 1 to 2 MGD: Cloudy or granular fluid.
Grade 3 to 4 MGD: Thick, toothpaste-like secretion, or no secretion at all (blocked).
Meibography
Advanced imaging systems use infrared light to photograph the Meibomian glands inside the eyelid. This allows the doctor to see the structure of the glands.
Dropout: The images reveal if glands have atrophied (died off). Once glands are lost, they cannot regenerate, which underscores the importance of early treatment.
Tear Film Break-Up Time (TBUT)
Fluorescein dye is instilled in the eye, and the patient is asked not to blink. The doctor times how long it takes for dry spots to appear on the cornea. A time of less than 10 seconds suggests instability likely caused by lipid deficiency from lid disease.
Medical and Surgical Management
Treatment strategies depend on whether the condition is infectious (stye), inflammatory (blepharitis), or structural (chalazion).
1. Management of Acute Styes
Most styes resolve on their own within a week.
Antibiotics: Topical antibiotic ointments (e.g., Erythromycin, Bacitracin) are prescribed to control the bacterial load.
Warm Compresses: Essential to increase blood flow and speed up the "pointing" and drainage of the abscess.
Avoidance: Patients must stop wearing makeup and contact lenses during an active infection to prevent spreading bacteria.
2. Surgical Removal of Chalazion (Incision and Curettage)
If a chalazion persists for several weeks despite conservative treatment, or if it is large enough to distort vision, surgical removal is the standard of care. This is a minor procedure performed in an outpatient clinical setting.
The Procedure:
Anesthesia: The eyelid is numbed with a local anesthetic injection. While the injection stings initially, the procedure itself is generally painless.
Clamp: A specialized chalazion clamp is applied. This flips the eyelid to expose the inner surface and controls bleeding.
Incision: A small vertical incision is made on the inner aspect of the eyelid (tarsal conjunctiva). This approach ensures there is no visible scar on the exterior skin.
Curettage: The contents of the cyst (granulomatous tissue) are scooped out using a curette. The cyst wall is also excised to prevent recurrence.
Recovery: Pressure is applied to stop bleeding. No sutures are usually required as the inner lining heals quickly. An eye patch may be worn for a few hours.
3. Advanced Treatments for Chronic Blepharitis/MGD
For patients with chronic Meibomian Gland Dysfunction where home remedies are insufficient, in-office procedures can help restore gland function.
Thermal Pulsation Systems (e.g., LipiFlow, iLux): These FDA-approved devices address the root cause of evaporative dry eye: the obstruction of the glands.
Mechanism: The devices apply therapeutic heat (approx. 42.5°C) to the inner and outer lids while simultaneously applying peristaltic massage.
Goal: The heat melts the hardened meibum (which has a melting point higher than body temperature), and the massage evacuates the stale oil. This "reboots" the glands, allowing them to secrete healthy, clear oil again.
Intense Pulsed Light (IPL) Therapy: Originally used in dermatology, IPL is highly effective for MGD, particularly in patients with Rosacea.
Mechanism: High-intensity light flashes are applied to the skin around the eyes.
Benefits:
Coagulates abnormal blood vessels (telangiectasia), reducing the delivery of inflammatory mediators to the eyelids.
Heats the glands to liquefy obstructions.
Reduces the population of Demodex mites and bacteria.
More information on IPL for Dry Eye.
Microblepharoexfoliation (BlephEx): This procedure acts like a deep dental cleaning but for the eyelids. A medical-grade microsponge spins at high speeds to physically scrub and remove the biofilm, scurf, and bacterial toxins from the eyelid margins that daily home hygiene might miss.
Home Remedies and Daily Hygiene Protocols
The most critical aspect of managing Blepharitis and MGD is patient compliance with daily hygiene. Much like brushing teeth to prevent plaque, eyelid hygiene prevents the buildup of biofilm and gland blockage.
The "Heat and Squeeze" Protocol
Physics dictates that the hardened oil in the glands must be melted before it can be expressed.
Heat (The Compress):
Use a microwaveable eye mask (bead or gel) rather than a wet washcloth. Washcloths lose heat too quickly.
Apply to closed eyes for 10 full minutes. The heat needs time to penetrate the skin and muscle to reach the tarsal plates where the glands reside.
Target temperature is roughly 40 to 45°C (warm, not scalding).
Massage (The Expression):
Immediately after removing the mask (while the oil is liquid), gently massage the eyelids.
Look up and roll a finger or cotton bud upwards on the lower lid.
Look down and roll downwards on the upper lid.
This mechanical action forces the liquefied oil out of the gland openings.
Cleanse (The Scrub):
After expressing the oil, the lid margins must be cleaned to remove the debris and bacteria.
Lid Wipes: Pre-moistened pads containing Tea Tree Oil (specifically the active ingredient Terpinen-4-ol) are excellent for killing Demodex mites.
Hypochlorous Acid Spray: A natural, gentle antimicrobial spray that neutralizes toxins and kills bacteria without stinging or harsh chemicals.
Baby Shampoo: Historically recommended, but now considered less ideal than dedicated lid cleansers as detergents can strip the tear film's lipid layer.
Dietary and Lifestyle Modifications
Omega-3 Fatty Acids: Clinical studies suggest that a diet rich in Omega-3s (EPA and DHA) helps improve the quality of meibum, making it less viscous and prone to clogging. Sources include salmon, sardines, flaxseed, or high-quality supplements.
The 20-20-20 Rule: In the digital age, we blink less frequently when staring at screens. This "incomplete blinking" causes the meibomian glands to stagnate. Every 20 minutes, look 20 feet away for 20 seconds and perform several hard, complete blinks to milk the glands.
Cosmetic Safety: Avoid applying eyeliner to the "waterline" (the inner rim of the eyelid posterior to the lashes). This practice physically caps the gland orifices, guaranteeing blockage over time.
Potential Complications of Neglect
Ignoring chronic eyelid inflammation can lead to downstream ocular health issues:
Madarosis: The permanent loss of eyelashes due to damage to the hair follicles.
Trichiasis: Misdirected growth of eyelashes. Scarring can cause lashes to turn inward, scratching the sensitive cornea with every blink.
Corneal Ulcers (Marginal Keratitis): Hypersensitivity to Staphylococcal toxins can cause white spots and ulcers on the periphery of the cornea, which are painful and can scar.
Permanent Dry Eye: Once Meibomian glands atrophy (die), they cannot be restored. This leads to permanent, lifelong dry eye requiring constant artificial tear use.
Important Medical Notice: This information provides general educational content about refractive errors and should not replace professional medical advice. For personalized assessment and treatment recommendations, please schedule a consultation with our eye care specialists. All vision correction methods including spectacles, contact lenses, and surgical procedures carry risks and limitations. Contact lenses carry risks of infection and corneal complications. Surgical corrections carry risks including infection, vision loss, need for additional procedures, and in rare cases permanent blindness. All options should be thoroughly discussed with a qualified ophthalmologist.
Licensed Healthcare Service: Our clinic operates in accordance with healthcare regulations. For questions about our services or to book an appointment, please visit our contact page or call during operating hours. For medical emergencies, contact emergency services immediately.
When to Seek Professional Care
Chronic inflammation of the eyelid margins disrupts the tear film's protective oil layer, causing persistent discomfort, crusty discharge, and unstable vision that worsens without proper lid hygiene and professional management. Please visit the doctor if you have any of the following symptoms:
Persistent morning crusting or matted eyelashes
Gritty sandy sensation despite no foreign objects
Red inflamed eyelid rims lasting several weeks
Painful tender lumps appearing on eyelid edges
Blurred vision that temporarily clears after blinking
Prompt consultation with an ophthalmologist enables accurate diagnosis of blepharitis, styes, or chalazia, preventing permanent gland loss and complications through targeted treatments and hygiene protocols.

