The Complete Patient Guide to Corneal Health: Conditions, Surgery, and Rehabilitation
The human eye is often compared to a camera, and the cornea acts as the camera's lens cover. It is the transparent, dome-shaped tissue that forms the front part of the eye. While it appears fragile, the cornea is a highly organized and resilient structure that serves two critical functions: it shields the rest of the eye from germs, dust, and other harmful matter, and it acts as the eye's outermost lens, controlling and focusing the entry of light into the eye. In fact, the cornea contributes between 65-75% of the eye's total focusing power.
Because the cornea is the window through which we see the world, keeping it clear and healthy is vital for good vision. Unlike most tissues in the body, the cornea contains no blood vessels (it is avascular). To remain transparent, it must stay free of blood vessels and receive oxygen directly from the air and nutrients from the tear fluid and the aqueous humor (the fluid inside the eye).
When the cornea is damaged by injury, infection, or hereditary disease, it can become swollen, scarred, or distorted. This damage prevents light from focusing properly on the retina, resulting in visual impairment ranging from mild blurriness to severe blindness.
This comprehensive guide explores the anatomy of the cornea, common pathologies such as Pterygium and Corneal Oedema, and the evolution of Corneal Transplantation techniques used to restore sight.
Anatomy of the Cornea: Understanding the Layers
To understand corneal conditions and their treatments, it is helpful to understand the structure of the cornea itself.
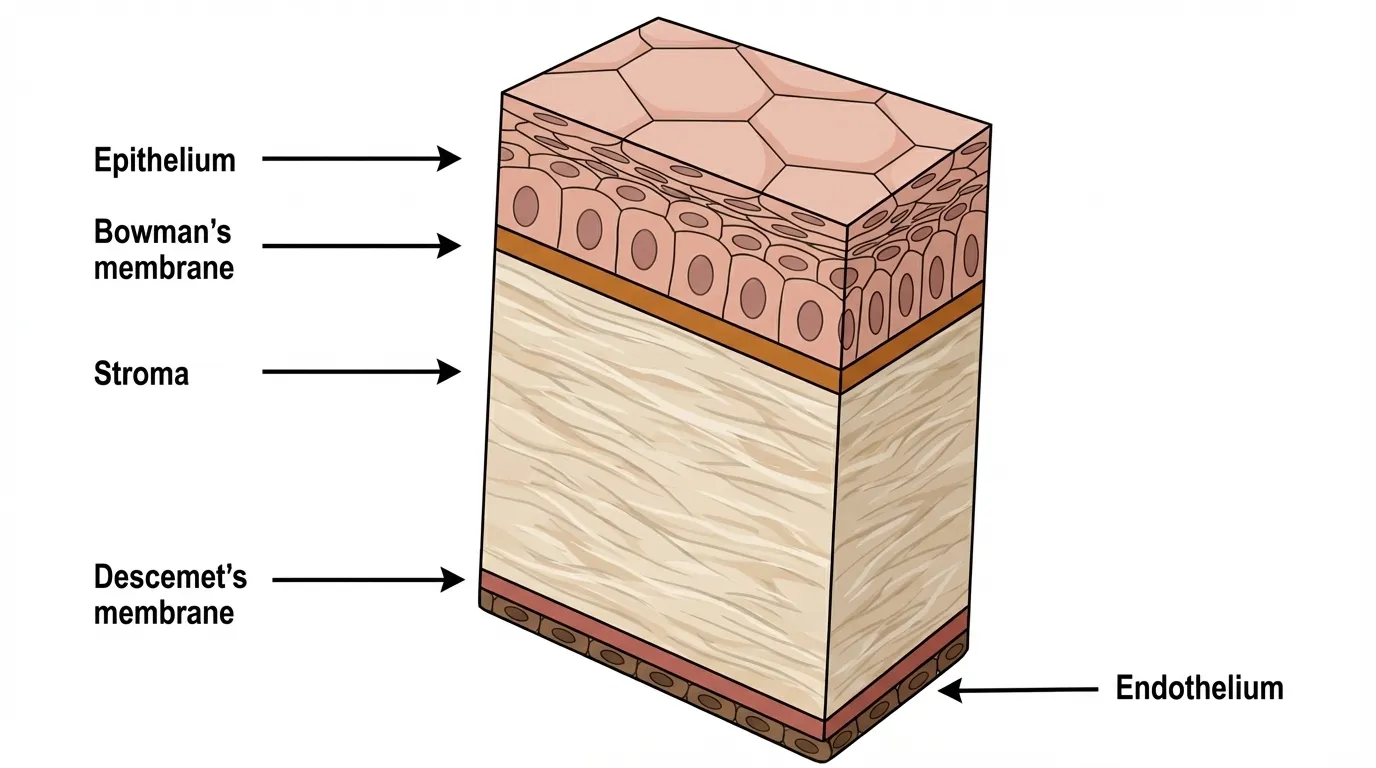
The cornea is less than 1mm thick but is composed of five distinct layers. Modern surgical techniques often target specific layers to preserve as much of the natural eye as possible.
Epithelium: The outermost layer. It functions as a barrier against dirt and bacteria and absorbs oxygen and nutrients from tears. It has remarkable regenerative properties; superficial scratches here often heal within days without scarring.
Bowman's Layer: A tough sheet of tissue composed of collagen. If injury penetrates this layer, it can result in permanent scarring.
Stroma: The thickest layer, making up about 90% of the cornea. It consists primarily of water and collagen fibers arranged in a precise, regular pattern to ensure transparency.
Descemet's Membrane: A thin but strong sheet of tissue that serves as a protective barrier against infection and injury. It acts as the basement membrane for the endothelial cells.
Endothelium: The single, innermost layer of cells. These cells are the cornea's "pump." They pump excess fluid out of the stroma. Without this pumping action, the stroma would absorb water, swell, and become hazy (oedema). Crucially, endothelial cells do not regenerate; once destroyed, they are lost forever.
What is a Pterygium?
A pterygium (plural: pterygia) is a pinkish, triangular, fleshy growth of the conjunctiva-the thin membrane covering the white part of the eye (sclera). While the word "growth" often causes alarm, a pterygium is a benign (non-cancerous) lesion. However, its benign nature does not mean it is harmless.
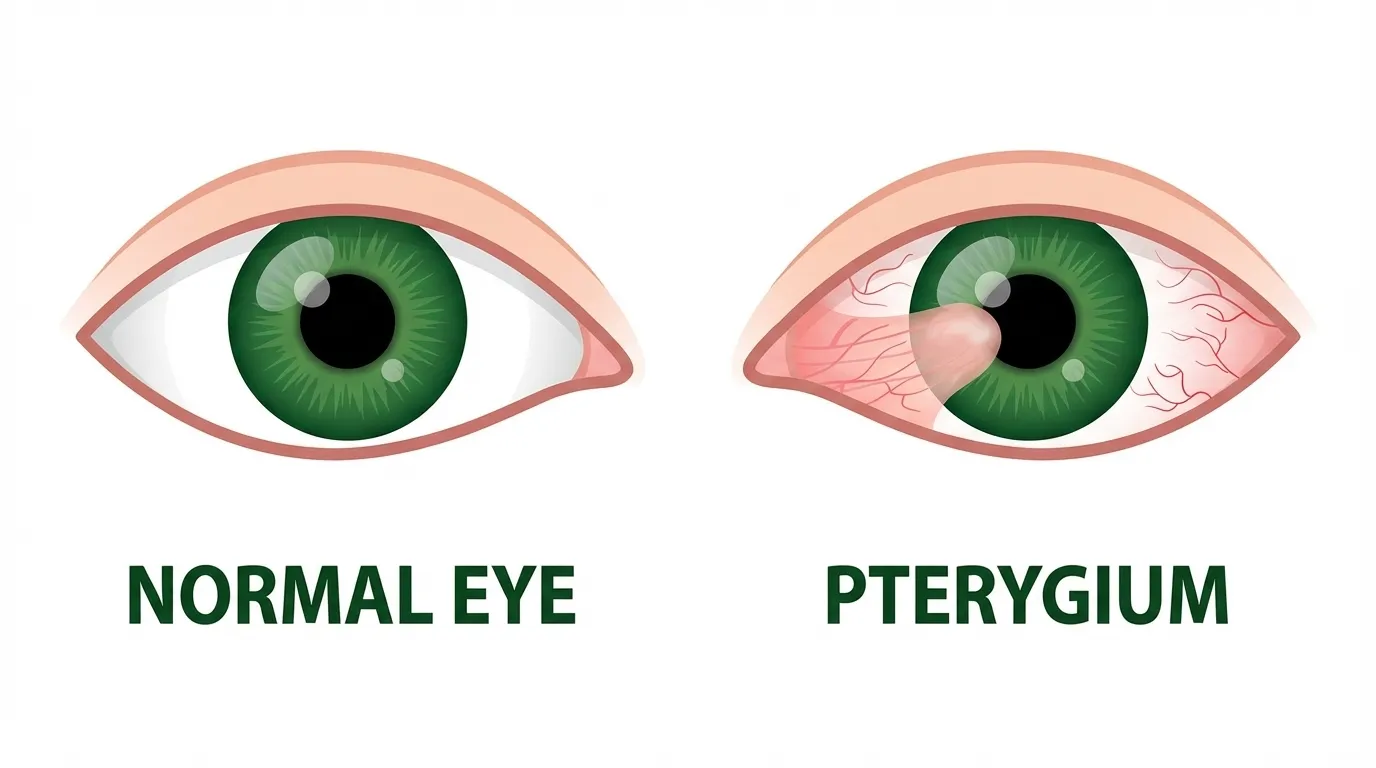
A pterygium typically starts on the conjunctiva near the nose and progressively grows horizontally toward the iris (the colored part of the eye). In its advanced stages, it encroaches onto the cornea itself. As it invades the corneal tissue, it physically pulls and distorts the corneal shape, causing astigmatism and blurred vision. In extreme, untreated cases, the fleshy tissue can grow entirely over the pupil, blocking light entry and causing profound vision loss.
Causes and Risk Factors: The "Surfer's Eye"
The exact pathogenesis of pterygium is multifactorial, but epidemiological studies strongly link it to environmental exposure. It is frequently referred to as "Surfer's Eye" because it affects populations who spend significant time outdoors.
Ultraviolet (UV) Radiation: This is the single most significant risk factor. People living near the equator have a higher prevalence due to intense, year-round sun exposure. UV light triggers oxidative stress and genetic changes in the conjunctival cells, prompting abnormal growth.
Environmental Irritants: Chronic exposure to wind, dust, sand, and smoke dries out the eye and causes micro-trauma, encouraging tissue proliferation.
Dry Eye Syndrome: A lack of protective tear film increases friction and inflammation, which may accelerate pterygium development.
For detailed research on the role of ultraviolet radiation in pterygium pathogenesis, extensive literature is available through the National Institute of Health.
Symptoms and Diagnosis
In the early stages (sometimes called a pinguecula before it invades the cornea), the condition may be asymptomatic other than the visible yellowish or pink bump. As it matures, symptoms include:
Chronic Redness: The growth contains its own blood vessels, leading to a persistently bloodshot appearance.
Foreign Body Sensation: A gritty feeling, as if sand is trapped in the eye.
Dryness and Itch: The elevated growth disrupts the even spread of the tear film.
Visual Disturbance: As the pterygium warps the corneal curvature, patients may notice their vision becoming blurred or double.
Diagnosis is typically clinical, performed by an eye care professional using a Slit-Lamp Bio-microscope. Additional diagnostics like Keratometry (measuring corneal curvature) and Anterior Segment Photography are used to document the size of the growth and the degree of astigmatism it is inducing.
Treatment Strategies
Medical Management
If the pterygium is small and not inducing astigmatism, surgical intervention may not be immediately necessary. Conservative management focuses on symptom relief:
Lubrication: Preservative-free artificial tears help maintain the tear film and reduce friction.
Anti-inflammatories: A short course of steroid eye drops may be prescribed during flare-ups to reduce redness and swelling.
Surgical Excision with Conjunctival Autograft
When the pterygium causes persistent discomfort, threatens vision, or presents a significant cosmetic concern, surgical removal is indicated. Historical methods of simply cutting off the growth (bare sclera technique) resulted in high recurrence rates, with the growth returning-often more aggressively-in up to 50% of cases.
Modern ophthalmology employs Pterygium Excision with Conjunctival Autografting, which significantly reduces the risk of recurrence.
Excision: Under local anaesthesia, the surgeon carefully peels and removes the abnormal tissue from the cornea and sclera.
Harvesting: A healthy piece of conjunctiva is harvested from underneath the patient's own upper eyelid (an area protected from UV damage).
Grafting: This healthy tissue is moved to the site where the pterygium was removed. It acts as a physiological barrier, preventing the abnormal tissue from growing back.
Fibrin Glue: Instead of traditional sutures which can cause irritation, many surgeons now use biological fibrin glue to attach the graft. This technique reduces post-operative pain and speeds up recovery.
Understanding the Condition
Corneal Oedema is the swelling of the cornea caused by the retention of fluid. As mentioned in the anatomy section, the corneal endothelium is responsible for pumping fluid out of the stroma to keep it clear. If these pump cells are damaged or decrease in number, fluid accumulates. The cornea thickens and loses its transparency, similar to a camera lens steaming up.
Primary Causes
1. Fuchs' Endothelial Dystrophy
This is a hereditary condition where endothelial cells slowly deteriorate and die off earlier than normal. It typically affects both eyes and is more common in women than men. As the cell count drops below a critical threshold, the pump function fails, leading to oedema. Research shows that Fuchs' dystrophy is the most common corneal endothelial dystrophy, affecting millions worldwide.
2. Surgical Trauma (Bullous Keratopathy)
Any intraocular surgery, such as cataract surgery or glaucoma surgery, creates stress on the corneal endothelium. While rare, eyes with borderline endothelial health may not recover from the surgical trauma, leading to persistent swelling known as Pseudophakic Bullous Keratopathy.
3. Glaucoma and Inflammation
Acute spikes in eye pressure (glaucoma) can overwhelm the endothelial pumps. Similarly, chronic inflammation (uveitis) can attack these delicate cells.
Symptoms of Corneal Oedema
Morning Blurriness: Vision is typically worse upon waking. This is because when the eyes are closed during sleep, no evaporation occurs, and fluid builds up. As the day progresses and the eyes open, evaporation helps draw some fluid out, slightly clearing vision.
Halos: Patients often report seeing rainbow-colored rings around streetlights or car headlights.
Pain (Bullous Keratopathy): In advanced stages, fluid accumulates on the surface epithelium, forming small blisters or "bullae." If these blisters rupture, it exposes sensitive corneal nerves, causing severe, sharp pain and increasing the risk of infectious ulcers.
The Evolution of Corneal Transplants
When conservative treatments (such as hypertonic saline drops to draw out fluid) fail, or when scarring is permanent, Corneal Transplantation (Keratoplasty) is the gold standard for visual rehabilitation.
Singapore has established itself as a regional leader in corneal transplantation, with institutions like the Singapore National Eye Centre (SNEC) and the Singapore Eye Bank (SEB) ensuring high standards of donor tissue quality.
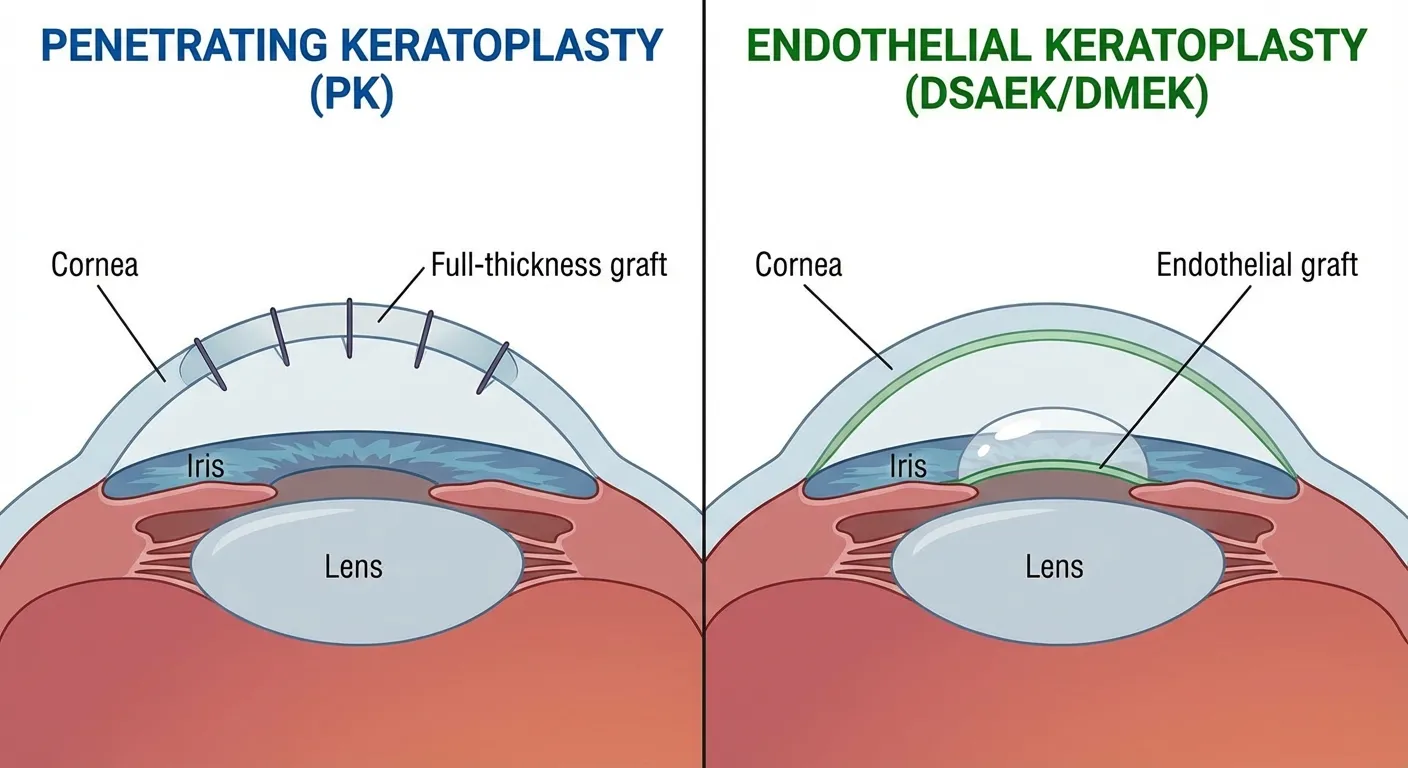
1. Penetrating Keratoplasty (PK) - The Traditional Approach
For decades, PK was the only option. It involves removing the entire central thickness of the diseased cornea (all 5 layers) and stitching a full-thickness donor cornea in its place.
Indications: Severe trauma, full-thickness scars, or combined stromal and endothelial disease.
Drawbacks: It requires multiple sutures (stitches), which remain in the eye for months or years. These sutures can induce significant astigmatism, and the recovery of vision is slow (up to 12 months). There is also a higher risk of graft rejection since there is more foreign tissue involved.
2. Anterior Lamellar Keratoplasty (ALK)
This technique is used when the disease is limited to the front layers of the cornea (e.g., scars from infections or keratoconus), but the patient's inner endothelium is healthy.
The Procedure: The surgeon removes only the diseased front layers and keeps the patient's own back layers intact. The donor tissue is then sutured on top.
Benefits: Because the patient retains their own endothelial pump cells, the risk of endothelial rejection is virtually eliminated. This ensures the graft can last a lifetime.
3. Endothelial Keratoplasty (DSAEK & DMEK)
This represents a paradigm shift in treating corneal oedema and Fuchs' dystrophy. Instead of replacing the whole cornea, surgeons replace only the damaged back layer. This is often described as "keyhole" corneal surgery.
DSAEK (Descemet Stripping Automated Endothelial Keratoplasty): A thin layer of donor tissue (containing the endothelium and a sliver of stroma) is transplanted.
DMEK (Descemet Membrane Endothelial Keratoplasty): An even thinner layer-just the membrane and the cells-is transplanted. This is the most anatomically correct repair possible.
The Procedure: Through a micro-incision, the donor tissue is rolled up and inserted into the eye. An air bubble is injected to press the tissue against the patient's cornea until it naturally adheres. No sutures are needed on the cornea itself.
Innovation Highlight: Surgeons in Singapore helped pioneer the EndoGlide, a device designed to insert the donor tissue safely without damaging the delicate cells. This has improved success rates globally.
Benefits:
Rapid Recovery: Vision can be restored in weeks rather than months.
Structural Integrity: The eye remains stronger and more resistant to injury than after PK.
Minimal Astigmatism: Since no tight sutures distort the cornea, the visual quality is often superior.
Recent research comparing ten-year outcomes shows that while DMEK and DSAEK provide faster visual recovery, each technique has distinct advantages depending on patient circumstances.
4. Artificial Corneas (Keratoprosthesis)
For patients with severe ocular surface disease (e.g., chemical burns or Stevens-Johnson syndrome) where a human donor transplant would almost certainly fail, artificial options exist.
Osteo-Odonto-Keratoprosthesis (OOKP): Also known as "tooth-in-eye" surgery. This complex, multi-stage procedure uses the patient's own tooth and bone to support an artificial plastic lens. It is a sight-saving procedure of last resort.
Boston Keratoprosthesis: An artificial cornea made of clear plastic and titanium, used for patients with multiple failed human transplants.
Pre-Operative Assessment
Before surgery, patients undergo a rigorous battery of tests:
Blood Tests & ECG: To ensure fitness for anaesthesia.
Biometry: To measure the eye's dimensions.
Viral Screening: To ensure no active infections.
Medication Review: Patients on blood thinners (e.g., aspirin, warfarin) may need to pause these medications to prevent intraocular bleeding.
Risks of Corneal Surgery
Graft Rejection: The human body may identify the donor cornea as "foreign" and attack it. Symptoms include the RSVP signals: Redness, Sensitivity to light, Vision drop, and Pain. Unlike organ transplants, corneal rejection can often be reversed with steroid drops if caught early.
Infection (Endophthalmitis): A rare but potentially blinding infection of the internal eye fluids.
Glaucoma: Post-operative pressure spikes are common and must be managed with drops or oral medication to prevent optic nerve damage.
Graft Detachment: In DSAEK/DMEK, the air bubble may fail to hold the graft in place, requiring a "re-bubbling" procedure in the operating theatre.
Refractive Errors: High astigmatism may persist, requiring glasses or contact lenses for optimal vision.
Anaesthesia
Surgeries are typically performed under General Anaesthesia (where the patient is asleep) or Regional/Local Anaesthesia (where the eye is numbed with an injection, and the patient is sedated). The choice depends on the patient's general health and the complexity of the procedure.
Immediate Post-Op Care
Eye Shield: A plastic shield is worn at night to prevent accidental rubbing or pressure on the eye while sleeping.
Positioning: For DSAEK/DMEK patients, lying flat on the back (supine) is often required for the first 24-48 hours to ensure the air bubble supports the graft.
Medications: A regimen of antibiotic drops (to prevent infection) and steroid drops (to prevent rejection/inflammation) is mandatory. In transplant cases, steroid drops may be tapered slowly over months or even years.
Long-Term Eye Health and Remedies
UV Protection: To prevent the recurrence of pterygium or damage to the new graft, patients must wear sunglasses with 100% UV protection when outdoors. Wide-brimmed hats are also recommended.
Lubrication: Keeping the ocular surface moist is crucial. Preservative-free lubricants should be used liberally, especially in air-conditioned environments.
Hygiene: Patients must practice strict hygiene, washing hands before touching the eye area or administering drops.
Regular Monitoring: Annual or bi-annual checks are essential for transplant patients for the rest of their lives to detect subtle signs of rejection or glaucoma.
Visual Rehabilitation
Visual recovery varies by procedure.
Pterygium Surgery: Vision usually stabilizes within 2-4 weeks.
DSAEK/DMEK: Functional vision often returns within 1-3 months.
PK/DALK: Visual stabilization can take up to 12 months due to suture adjustment.
Corrective Lenses: Once the cornea has healed, remaining refractive errors can be corrected with spectacles or rigid gas-permeable (RGP) contact lenses, which provide a smooth optical surface over irregular corneas.
For further reading on the outcomes of corneal transplantation and visual rehabilitation, extensive patient resources and statistical data are available through the Cornea Research Foundation.
Important Medical Notice: This information provides general educational content about corneal health and should not replace professional medical advice. For personalized assessment and treatment recommendations, please schedule a consultation with our eye care specialists. All vision correction methods including spectacles, contact lenses, and surgical procedures carry risks and limitations. Contact lenses carry risks of infection and corneal complications. Surgical corrections carry risks including infection, vision loss, need for additional procedures, and in rare cases permanent blindness. All options should be thoroughly discussed with a qualified ophthalmologist.
Licensed Healthcare Service: Our clinic operates in accordance with healthcare regulations. For questions about our services or to book an appointment, please visit our contact page or call during operating hours. For medical emergencies, contact emergency services immediately.
When to Seek Professional Care
A transparent, dome-shaped tissue at the front of the eye can become damaged by injury, infection, or hereditary disease, affecting vision quality and clarity. Please visit the doctor if you have any of the following symptoms:
Persistent redness or bloodshot appearance in eyes
Gritty sensation as if sand trapped inside
Vision becoming progressively blurred or distorted
Rainbow-coloured halos around lights at night
Morning blurriness that improves throughout the day
Timely corneal assessment and modern surgical interventions can restore visual clarity, prevent complications, and preserve long-term sight when conservative treatments prove insufficient.