Iris Conditions: Understanding Inflammation and Iritis
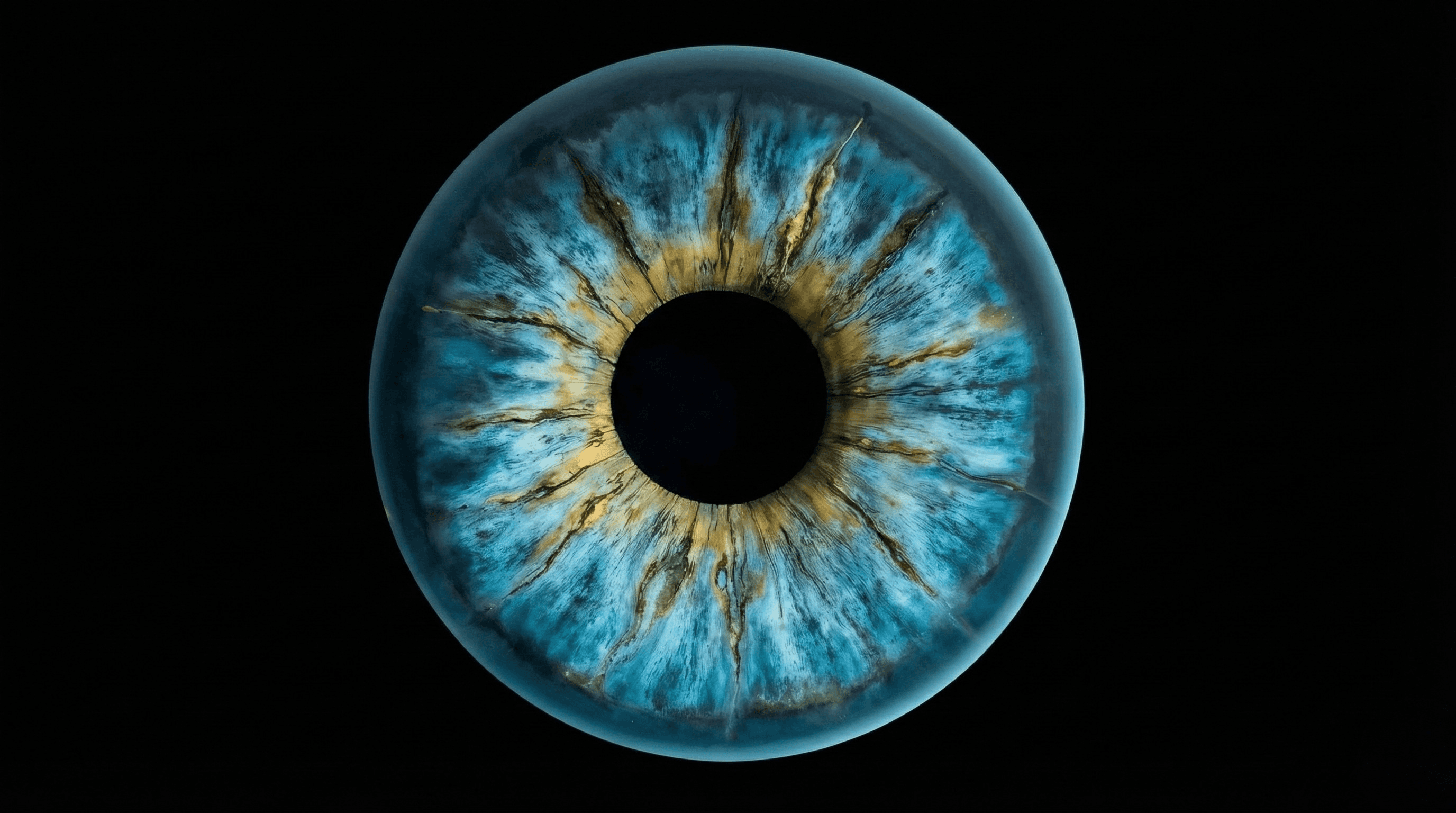
The iris is the colored part of your eye that surrounds the pupil, controlling how much light enters through the pupil opening to reach the retina. Made up of muscular fibers, the iris automatically adjusts your pupil size, making it smaller in bright light and larger in dim conditions to help you see clearly. When the iris becomes inflamed, a condition known as iritis or anterior uveitis develops, which can cause pain, redness, and potentially vision problems if not promptly treated. Understanding iris inflammation and seeking timely medical care are important for protecting your vision and preventing complications.
Important: Iritis requires prompt medical treatment. Delayed or inadequate treatment may result in permanent vision loss. All medications used to treat iritis carry potential side effects that should be discussed with your ophthalmologist.
What Is Iritis (Anterior Uveitis)?
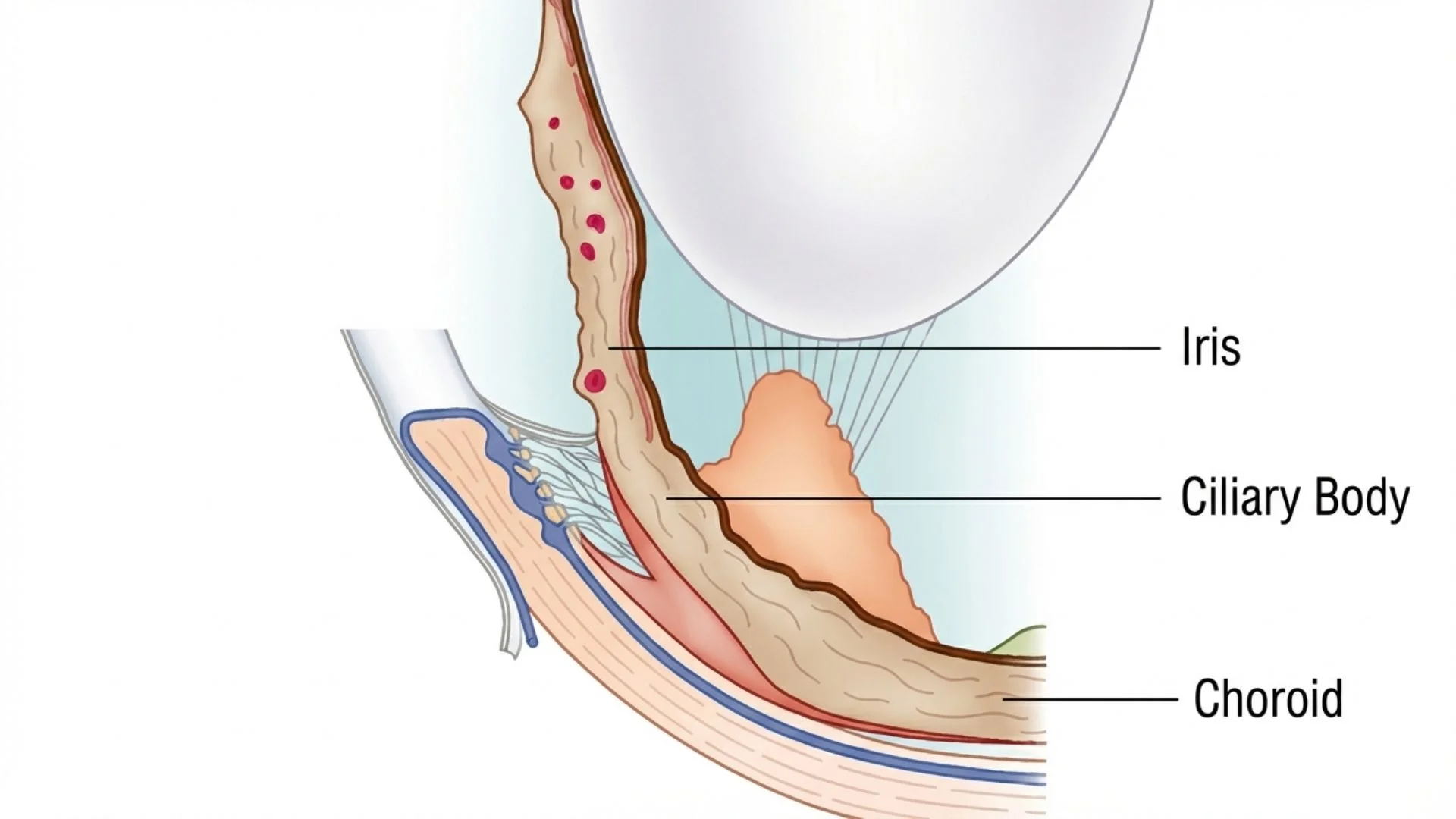
Iritis, also called anterior uveitis, is inflammation affecting the iris and the front portion of the uvea, which is the middle vascular layer of the eye between the sclera and retina. The uvea consists of three parts: the iris at the front, the ciliary body in the middle, and the choroid at the back. When inflammation specifically affects the iris and surrounding anterior structures, it is termed iritis or anterior uveitis.
This condition represents one of several types of uveitis, classified based on which part of the uvea is affected. Anterior uveitis affects the iris at the front of the eye and is the most common type. Intermediate uveitis affects the ciliary body and vitreous gel in the middle of the eye. Posterior uveitis affects the retina and choroid at the back of the eye. Panuveitis affects all parts of the uvea from front to back.
Iritis typically develops suddenly and most often affects only one eye, though both eyes can be affected simultaneously or sequentially. It may occur as an acute episode that resolves with treatment, or it can become chronic with recurring attacks. Approximately one in three patients will experience recurrent episodes throughout their lifetime.
Understanding Inflammation in the Eye
Inflammation is normally your immune system's protective response to injury or infection. When inflammation occurs in the eye, your immune system may be fighting an actual eye infection, but it can also mistakenly attack healthy eye tissue in autoimmune conditions. This inappropriate immune response causes the symptoms and complications associated with iritis.
The inflammation in iritis can lead to various changes within the eye, including accumulation of inflammatory cells in the anterior chamber, deposits on the back surface of the cornea, and adhesions between the iris and lens. These changes interfere with normal eye function and can cause permanent damage if not adequately treated.
Symptoms of Iritis
Iritis symptoms usually develop quickly, often over a few hours to several days. Recognizing these symptoms early and seeking prompt evaluation is important for preventing complications and preserving vision.
Acute Iritis Symptoms
The characteristic symptoms of acute iritis include eye pain with aching or throbbing in the affected eye or brow area, often worsening in bright light. Photophobia or severe light sensitivity makes it difficult to tolerate normal lighting conditions. Eye redness is typically pronounced, particularly concentrated around the iris rather than diffusely across the entire eye surface.

Blurred vision may range from mild to severe, and the affected pupil may appear unusually small, irregularly shaped, or react poorly to light compared to the unaffected eye. Additional symptoms include excessive tearing and headache that may extend beyond the eye to the surrounding head area.
These symptoms typically worsen when trying to read or focus on near objects, and the pain intensifies in brightly lit environments. Many patients find relief by wearing dark glasses or staying in dimly lit rooms during acute episodes.
Chronic Iritis Symptoms
In chronic anterior uveitis, the presentation may be quite different from acute attacks. The eye may no longer appear red, pain may be minimal or absent, and vision may be blurred without other obvious symptoms. Some patients experience no noticeable symptoms at all, with inflammation detected only during routine eye examinations. This subtle presentation makes chronic iritis particularly concerning, as ongoing inflammation can cause cumulative damage without obvious warning signs.
Warning Signs Requiring Immediate Attention
Seek immediate evaluation from an eye care specialist if you experience sudden onset of eye pain with redness, severe sensitivity to light, rapid vision deterioration, eye pain that worsens when pressing gently on the eyelid, or any combination of these symptoms, even if mild. Early treatment may improve outcomes and reduce the risk of complications, though complications can still occur despite prompt treatment.
Causes and Risk Factors
In more than half of iritis cases, no specific cause can be identified. When an underlying cause is found, it often relates to systemic conditions, infections, or genetic factors.
Autoimmune and Inflammatory Conditions
Various autoimmune disorders are associated with increased risk of developing iritis, including ankylosing spondylitis, a type of inflammatory arthritis primarily affecting the spine. Reactive arthritis develops in response to infections elsewhere in the body. Sarcoidosis causes inflammation in multiple organs including the eyes. Inflammatory bowel disease, including Crohn's disease and ulcerative colitis, can trigger ocular inflammation. Behçet's disease is a rare disorder causing blood vessel inflammation throughout the body. Other associated conditions include juvenile idiopathic arthritis, psoriasis, lupus, and multiple sclerosis.
Infections
Both infectious organisms and the body's response to infections can trigger iritis. Viral infections including herpes simplex, herpes zoster (shingles), and cytomegalovirus can cause iritis. Bacterial infections such as tuberculosis, syphilis, and Lyme disease may trigger inflammation. Fungal and parasitic infections including histoplasmosis and toxoplasmosis are less common causes. In infection-related cases, treating the underlying infection is essential alongside managing the eye inflammation.
Genetic Factors
Certain genetic markers increase susceptibility to iritis. The HLA-B27 gene is particularly significant, with individuals carrying this gene having substantially higher risk of developing anterior uveitis. Not everyone with this gene develops iritis, but its presence is a recognized risk factor, especially when combined with conditions like ankylosing spondylitis.
Eye Trauma and Other Risk Factors
Physical injury to the eye from blunt trauma, puncture wounds, chemical or thermal burns, or surgical trauma from previous eye procedures can trigger iritis. Post-traumatic iritis may develop immediately following injury or appear days to weeks later. Certain medications can occasionally cause iritis as a side effect, though this is relatively uncommon. Additional risk factors include smoking, previous episodes of iritis, and age, as iritis is most common in people between ages 20 and 60.
Diagnostic Procedures
Prompt and accurate diagnosis is essential for initiating appropriate treatment and preventing complications. Your eye doctor will perform several examinations and tests to confirm iritis and investigate potential underlying causes.
Clinical Eye Examinations
Your ophthalmologist begins by examining external eye structures using a penlight or similar device, assessing the pattern and location of redness, pupil size, shape, and reaction to light, and response to gentle pressure. Visual acuity testing using an eye chart measures how inflammation affects your visual clarity. Measuring the intraocular pressure inside your eye is important because iritis can cause abnormal eye pressure. Elevated pressure requires additional management to prevent glaucoma damage, while abnormally low pressure may indicate severe inflammation.
Slit-lamp biomicroscopy is the primary diagnostic tool for confirming iritis. This specialized microscope illuminates and magnifies eye structures, allowing detailed examination of inflammatory cells floating in the anterior chamber fluid, protein accumulation appearing as hazy fluid, keratic precipitates (deposits on the cornea's back surface), posterior synechiae (adhesions where iris sticks to lens), iris color changes or structural abnormalities, and signs of complications such as cataract formation.
Before the slit-lamp examination, your doctor may instill dilating eye drops to widen your pupil, allowing better visualization of posterior structures and ensuring no intermediate or posterior uveitis is present. Your vision will be temporarily blurred for approximately two to three hours following dilation.
Additional Diagnostic Testing
Depending on your symptoms, medical history, and examination findings, additional tests may be necessary to identify underlying causes. Blood tests may be recommended if you have had multiple episodes, both eyes have been affected, you have symptoms suggesting a systemic condition, or no obvious cause is identified in recurrent cases. Blood tests can detect inflammatory markers, antibodies associated with specific diseases, genetic markers like HLA-B27, and evidence of infections. Chest X-rays or other imaging may be ordered if conditions like sarcoidosis or tuberculosis are suspected.
Treatment Procedures for Iritis
Iritis treatment aims to reduce inflammation, relieve pain, prevent complications, and preserve vision. Prompt treatment is important, as untreated or inadequately treated iritis may lead to vision loss that can be permanent.
Important Treatment Information: All medications used to treat iritis carry potential side effects and risks. Corticosteroids may cause elevated eye pressure, cataracts, increased infection risk, and other complications. Treatment effectiveness varies by individual, and some patients may not respond to initial treatment. All treatment risks and benefits should be discussed with your ophthalmologist.
Medication-Based Treatment
Corticosteroid Eye Drops
Steroid eye drops form the cornerstone of iritis treatment. These medications effectively reduce inflammation in the eye. Treatment usually begins with frequent application, sometimes hourly initially for severe inflammation, and gradually decreases in frequency as inflammation resolves. The specific steroid formulation and dosing schedule depend on inflammation severity and location. It is important to follow the prescribed tapering schedule rather than stopping suddenly, as abrupt discontinuation can cause inflammation to rebound.
Cycloplegic and Mydriatic Eye Drops
Dilating drops serve multiple important functions in iritis treatment. By relaxing the iris muscles and dilating the pupil, these drops significantly reduce pain associated with iris inflammation and muscle spasm. Keeping the pupil dilated prevents the iris from sticking to the underlying lens, and in some cases these drops can help separate mild adhesions that have already formed. Common dilating medications include cyclopentolate and atropine. While using these drops, your vision will be blurred, particularly for reading and near work, and you may experience increased light sensitivity. These effects are temporary and resolve once the drops are discontinued.
Pressure-Lowering Eye Drops
If inflammation or steroid treatment causes elevated intraocular pressure, additional drops to lower eye pressure may be prescribed. This is particularly important if you have a history of pressure elevation with previous episodes or if you have existing glaucoma. Untreated elevated pressure can damage the optic nerve, so monitoring and management are essential.
Systemic Treatment
If eye drops do not adequately control inflammation, or if inflammation is particularly severe, your doctor may prescribe oral corticosteroids or other immunosuppressive medications. These systemic treatments are particularly important when iritis is associated with an underlying systemic condition requiring treatment, eye drop treatment proves insufficient, both eyes are severely affected, or chronic or recurrent inflammation requires long-term management.
For iritis related to autoimmune conditions, medications that modify immune system function may be necessary. Managing these medications typically involves coordination between your ophthalmologist and a rheumatologist or other specialist familiar with your systemic condition. When iritis results from an infection, appropriate antimicrobial therapy must be administered alongside anti-inflammatory treatment.
Treatment Duration and Follow-Up
The duration of treatment varies depending on inflammation severity and individual response. Acute episodes typically resolve within six to eight weeks with appropriate treatment, though you will need to continue medication even after symptoms improve to ensure complete inflammation resolution. Regular follow-up appointments are essential for monitoring treatment response, adjusting medication dosages, checking for complications, ensuring complete resolution before discontinuing treatment, and detecting chronic inflammation that may persist without obvious symptoms.
Complications of Untreated or Poorly Managed Iritis

Without appropriate treatment, iritis may lead to complications that can cause permanent vision loss. Posterior synechiae, adhesions between the inflamed iris and underlying lens, can cause irregular pupil shape and block fluid circulation, leading to elevated pressure and secondary glaucoma. Glaucoma can develop through several mechanisms including inflammatory cells blocking drainage, extensive adhesions preventing fluid circulation, steroid-induced pressure elevation, or chronic inflammation damaging drainage structures.
Both inflammation itself and corticosteroid treatment can accelerate cataract development. Patients with chronic or recurrent iritis may develop cataracts. Inflammation can cause cystoid macular edema, swelling in the macula that causes blurred or distorted central vision which may be permanent. Chronic inflammation can cause band keratopathy, calcium deposits forming on the corneal surface creating opacity that may require surgical removal. Additional complications may include vitritis, retinitis, optic nerve damage, hypotony, and permanent vision loss. Some complications may occur despite appropriate treatment and careful management.
Living with Recurrent Iritis
Approximately one-third of patients experience recurrent episodes of iritis. Understanding how to manage this chronic condition and recognize recurrences early helps preserve vision and quality of life. Learn to recognize early warning signs including onset of eye discomfort or pain, increasing redness particularly around the iris, development of light sensitivity, vision changes or blurring, or any combination of familiar symptoms from previous episodes. If you suspect a recurrence, contact your eye care specialist immediately.
Self-treatment is discouraged because red eye symptoms can result from various conditions, some of which worsen with steroid use. The severity of each episode may differ, requiring adjusted treatment. Professional assessment ensures proper diagnosis and optimal management. During active inflammation, wear sunglasses to reduce light sensitivity, rest in a darkened room if symptoms are severe, take over-the-counter pain relief for discomfort, avoid driving if vision is blurred or you are using dilating drops, and limit activities requiring clear vision until inflammation resolves.
Prevention and Self-Care
While iritis often cannot be prevented, certain measures may reduce risk and support overall eye health. Studies demonstrate that smoking contributes to increased uveitis risk. If you smoke, discuss cessation strategies with your healthcare provider. If you have a systemic condition associated with iritis, work closely with your healthcare team to maintain optimal disease control. Wear appropriate eye protection during activities with injury risk, use quality sunglasses that block UVA and UVB rays, maintain good overall health through balanced nutrition and regular exercise, and practice stress management techniques.
When to Contact Your Doctor
Between episodes, contact your eye care team if you experience any symptoms suggesting iritis recurrence, vision changes including new floaters, halos around lights, or blurring, eye pain or discomfort, persistent redness, or any eye-related concerns. If you notice halos around lights and blurred vision, particularly upon waking, your eye pressure may be elevated and should be checked within a few days.
Conclusion
Iritis is a condition requiring prompt diagnosis and treatment to help preserve vision and reduce the risk of complications. While recurrences can occur, treatment options are available when properly administered. Understanding your condition, recognizing symptoms early, adhering to treatment regimens, and maintaining regular follow-up care are important steps in managing iritis.
If you develop symptoms of iritis or have concerns about eye inflammation, our ophthalmologists provide evaluation and treatment. We offer management of both acute and chronic inflammatory eye conditions.
Important Medical Disclaimer: This content provides general educational information about iris inflammation and iritis. It does not replace professional medical advice tailored to your individual circumstances. Treatment decisions must be based on comprehensive examination by a qualified ophthalmologist who can assess your specific situation and recommend appropriate management strategies. All treatments carry risks including infection, elevated eye pressure, cataracts, and in some cases permanent vision loss despite appropriate treatment.
Licensed Healthcare Service: For appointments, questions about our services, or concerns about iritis symptoms, please visit our contact page or call during business hours. For urgent eye symptoms including sudden eye pain, redness, or vision changes, seek immediate evaluation at an eye emergency department or contact emergency services.
When to Seek Professional Care
Inflammation of the iris causes pain, redness, and light sensitivity that requires prompt medical attention to prevent permanent vision damage. Please visit the doctor if you have any of the following symptoms:
Sudden eye pain with aching around brow area
Severe sensitivity to light or bright environments
Pronounced redness concentrated around the coloured iris
Blurred vision with unusually small irregular pupil
Eye pain worsening when pressing on eyelid
Immediate evaluation by an eye specialist ensures proper treatment, reduces complication risks, and helps preserve vision in acute and recurrent cases.