By Dr Ajeet Madhav Wagle, Medical Director and Senior Consultant Ophthalmologist, International Eye Cataract Retina Centre at Mount Elizabeth Medical Centre and Farrer Park Medical Centre, Singapore
Dry eye is one of the most common eye conditions that patients seek medical attention for from an eye specialist. The symptoms of dry eye can range from mild occasional discomfort in the eyes to severe debilitating symptoms such as blurry vision and eye pain that significantly affect one’s quality of life.
CAUSES OF DRY EYE
The normal tear film that covers the exposed surface of the eye is made up of three layers – 1) a thin inner mucus layer lining the eye surface, 2) a thin outer layer of oil or lipids exposed to the environment, and 3) a thick middle layer of aqueous or fluid sandwiched in between the inner mucus and outer lipid layers. Problems with any of these three important components of the tear film can lead to dryness of the eye.
Dry eye occurs because of inadequate or inefficient lubrication of the smooth outer surface of the eyeball. Dry eye can result from 1) a decreased quantity of tear fluid because of decreased tear fluid production, 2) increased tear fluid evaporation due to poor tear fluid quality or 3) a combination of the two factors.
Common causes for reduced tear production are ageing, hormonal changes, menopause, diabetes and autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus.
An increased tear evaporation may occur due to exposure to dry or windy environment, haze, excessive use of digital screens and cigarette smoking. As blinking of the eyes helps to resurface the eyeball with a fresh coat of tear fluid, an inability to close the eyelids properly can also result in dryness from excessive evaporation of tears.
Imbalance of tear fluid composition may occur because of improper functioning of the tiny oil secreting glands (called Meibomian glands) that line the eyelid margin. Contact lens wear, previous eye surgeries such as LASIK and use of certain oral medications can aggravate symptoms of dry eye as well.
SYMPTOMS OF DRY EYE
A variety of symptoms may be experienced by patients suffering from dry eye. Common symptoms include stinging, burning, scratchy or foreign body sensation, redness, sensitivity to light, intermittent blurry vision and tired eyes.
Interestingly, tearing is paradoxically a common symptom of dry eye. This tearing results from a reflex action that causes a sudden over production of the tear fluid by the body in response to persistent dryness in the eye.
DIAGNOSTIC TESTS FOR DRY EYE
Besides a thorough history of the symptoms and a comprehensive eye examination (including eyelid blinking pattern, eyelid margin and eyelash examination), targeted eye tests are essential for understanding the cause of the dry eye.
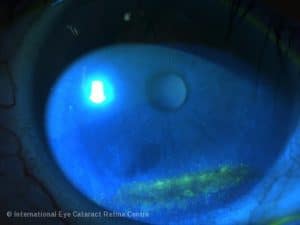
Dry eye tests are performed by an eye specialist in the clinic. These include tear break up time (TBUT) to measure tear film stability, eye surface staining (using fluorescein, rose Bengal or lissamine green dyes) to quantify the effect of dryness on the surface of the eye, Schirmer test to measure basal or reflex tear fluid production, tear fluid osmolarity and occasionally some other special blood tests to detect autoimmune diseases.
TREATMENT OF DRY EYE
Many patients self-treat dry eye with over-the-counter eye lubricants. However, it is important to understand that “one size does not fit all’. The treatment of dry eye needs to be customised to the cause and severity of the dry eye.
Mild dry eye can be managed with the use of preserved artificial tear substitutes, environmental modification and adoption of good visual habits while using digital screens.
Moderately severe dry eye requires preservative-free artificial tear substitutes, anti-inflammatory medications and eyelid care. In some patients, lacrimal punctal plugs may be recommended by your doctor to preserve the normal tear fluid within the eye.
Severe dry eye is treated with frequent application of preservative-free artificial tear substitutes, specially compounded autologous serum eye drops, anti-inflammatory eye drops and oral anti-inflammatory medications. Rarely, eye surgery may be required for treating severe dry eye.
A new treatment modality that has been introduced recently is transcutaneous electrical stimulation. In a recent study, it was found that transcutaneous electrical stimulation can improve patients’ dry eye, both subjectively and objectively, without any adverse effects.1

COMPLICATIONS OF DRY EYE
Fortunately, dry eye is not frequently associated with vision threatening complications. However, symptoms of dry eye can significantly affect one’s quality of life.
Dry eye increases the risk of developing “blood shot” eyes (subconjunctival haemorrhage), corneal abrasions and corneal infections.
As dry eye can result from a variety of causes, a thorough and targeted eye evaluation by an eye specialist is recommended to allow appropriate and individualised treatment. A casual evaluation without investigating for and treating all possible causes of the condition can leave patients frustrated with persistent symptoms.
Unfortunately, dry eye cannot be completely cured. However, most patients with dry eye are able to have their symptoms minimised with appropriate use of treatment regimens prescribed by their eye specialist. Regular eye checks are recommended to monitor the condition even if symptoms are well-controlled with the prescribed treatment.
REFERENCE
- Petrotii E, Sosello F, Fasolo A, et al. Transcutaneous periorbital electrical stimulation in the treatment of dry eye. British Journal of Ophthalmology 2017; 101:814-819.
