
Dr Joy Chan
MBBS(Singapore)(Gold Medallist) MRCS(Edinburgh) FAMS(Ophthalmology)(Singapore)
By Dr Joy Chan, Medical Director and Senior Consultant Ophthalmologist, International Eye Cataract Retina Centre at Mount Elizabeth Medical Centre and Farrer Park Medical Centre, Singapore
January is Glaucoma Awareness Month and it is fitting to start the year by raising awareness about a condition that is also known as the “silent thief of sight”.
WHAT IS GLAUCOMA?
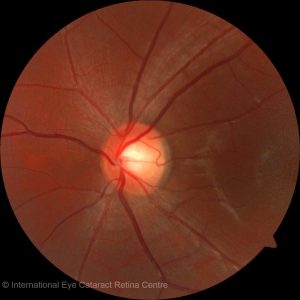
Glaucoma is a group of diseases that affects the optic nerve of the eye. Images perceived by the retina generate electrical signals that are carried via the optic nerve to the brain where they are interpreted. Hence, the optic nerve is a very important structure of the visual system and its health is critical to having good vision.
In glaucoma, the optic nerve is progressively damaged and this affects both its structure and function. Structural damage of the optic nerve can be seen by an ophthalmologist using special instruments to visualise the inside of the eye. Structural damage can be measured objectively with specialised tests that can be done in an ophthalmologist’s clinic.
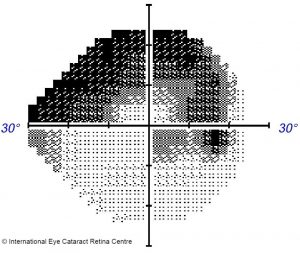
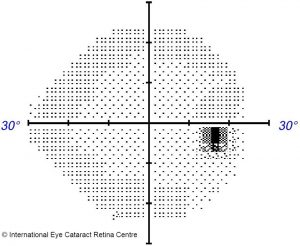
Functional damage to the optic nerve typically results in a loss of one’s peripheral vision, which can progress from mild loss to tunnel vision. Tunnel vision results from severe loss of peripheral vision such that only a small constricted circular tunnel-like field of central vision remains. Interestingly, although peripheral vision is very important, mild losses are usually not noticed by patients. For example, when you see something out of the corner of your eye (such as a car on the road), your instinct is to turn your head in the direction of the car, thereby bringing it into your central field of vision. Hence, if your peripheral vision is poor, you may not initially realise it.
The cause of the optic nerve damage is frequently (but not always) raised eyeball (or intraocular) pressure, and hence the strategy to treat glaucoma involves lowering the eyeball pressure. This is usually achieved with medications, but may also involve laser treatment or surgery.
Here’s one fact that is quite frightening – most cases of glaucoma have no symptoms! Normal eyeball pressure is about 12 to 21mmHg, and contrary to popular belief, eyeball pressure can be raised without pain or other symptoms. A patient usually only feels eye pain when the eyeball pressure is extremely elevated. Unfortunately, in most cases of glaucoma, eyeball pressure is raised but not to the extent that it causes pain, and optic nerve damage goes undetected until the late stage of the disease. Patients sometimes present with only tunnel vision remaining, and because optic nerve damage cannot be reversed, there is currently no way to restore their peripheral vision once lost.
THE IMPACT OF GLAUCOMA
Glaucoma has been identified by the World Health Organisation as a Priority Eye Disease. Its impact is significant as the number of persons estimated to be blind as a result of primary glaucoma is 4.5 million, accounting for slightly more than 12% of all global blindness.
In Singapore, the overall prevalence of glaucoma is 4% – meaning that in your lifetime, you have a 4% chance of developing glaucoma. Although the odds are in your favour, it is still a condition worth knowing about because it is potentially blinding and much of the visual loss can be prevented if detected early.
There are two common forms of glaucoma: open angle glaucoma and angle closure glaucoma.
OPEN ANGLE GLAUCOMA
Open angle glaucoma accounts for nearly half of all glaucoma cases in Singapore – 1.7% of the population have or will have this disease. Although this figure does not sound intimidating, what is worrisome is that this disease does not have symptoms in its early stages and many patients are diagnosed late for this reason.
In open angle glaucoma, the optic nerve at the back of the eye undergoes progressive damage. This is most often (but not always) due to high eyeball pressure. The condition does not cause pain or discomfort to the eye, and the patient is often unaware that he has glaucoma.
The result of optic nerve damage is visual field loss – a reduction in the patient’s peripheral vision. Peripheral vision is important in daily life – it allows us to safely cross roads or drive, for example, but early peripheral vision loss is usually not noticeable. A loss of central vision is often noticed by patients immediately, but loss of peripheral vision is much more subtle and can progress to severe loss before it is perceived by the patient.
As a result, open angle glaucoma is often diagnosed late, when significant peripheral field loss has occurred. Occasionally patients present when only tunnel vision remains, or worse, when the peripheral field is completely lost and the disease starts to affect central vision.
How is open angle glaucoma diagnosed? When patients present to an ophthalmologist, a detailed history and physical examination is performed. The eyeball pressure is measured – usually raised beyond 21mmHg in the case of open angle glaucoma. Signs that point to the disease – a characteristic “weak”, thinned-out appearance of the optic nerve, would make one suspicious of the disease. The disease is often confirmed on further testing where both structure and function of the nerve is tested. High-resolution optical coherence tomography (OCT) scans of the optic disc and the surrounding retinal nerve fibre layer can determine if there is any thinning of the nerve due to glaucoma, and Humphrey visual field (HVF) testing can map out areas of visual field loss.
Open angle glaucoma may be treated with eyedrops, laser therapy or surgery, depending on the severity of the disease.
ANGLE CLOSURE GLAUCOMA
The front of the eyeball is filled with a colourless fluid known as aqueous humour. It is continually being produced in the eye and drained from the eye through a drainage channel in the eye called the trabecular meshwork. In some patients, the part of the eye where the trabecular meshwork is located (known as the anterior chamber angle) is narrow, which can reduce the drainage of fluid from the eye. When pressure builds up in the eye as a result of this, angle closure glaucoma results.
Pressure build up can occur acutely and can build up to very high levels. This results in symptoms of eye pain, redness, blurred vision and headache. The patient may also experience nausea and vomiting.
Angle closure glaucoma is an emergency. When the eye pressure is dangerously high, the optic nerve located at the back of the eye can become damaged within a day or two. This damage is irreversible and the patient can permanently lose vision as a result.
How is this condition treated? In the acute situation, the priority is to lower the eye pressure as quickly as possible to reduce damage to the optic nerve. This is achieved using medications which are administered as eyedrops, oral pills or even injections. A laser surgery called laser iridotomy is performed to create an alternative channel for fluid to flow and prevent the build-up of pressure from occurring again. The laser surgery is usually also performed in the opposite eye as it is also at risk of developing angle closure glaucoma.
Patients with this condition sometimes suffer damage to the trabecular meshwork as a result of the high pressure, thus leading to chronic angle closure glaucoma. These patients often require life-long treatment with anti-glaucoma eyedrops or surgery.

THE IMPORTANCE OF EYE SCREENING
As glaucoma is often a disease without symptoms, it is important to go for regular eye screening to detect the disease at an early stage. This is so that treatment can be instituted in a timely manner, and visual loss can be minimised. If you are over the age of 40, or have a family member with the condition, it is a good idea to schedule a visit to an ophthalmologist to get yourself checked for glaucoma.

