Age-related macular degeneration (AMD), also known as age-related maculopathy, is the most common cause of severe irreversible vision loss among people over the age of 60 years in developed countries. It is the third most common cause of blindness worldwide after cataract and glaucoma.
Macular degeneration occurs when the macula ceases to function properly. Although the exact cause of macular degeneration is still unknown, the vast majority of macular degeneration is related to ageing, hence the term age-related macular degeneration. The risk of developing AMD increases with age.
Another common cause of macular degeneration is severe short-sightedness or myopia. This form of macular degeneration is called myopic macular degeneration.
- Older age
- Positive family history
- Female gender
- High blood pressure
- Heart disease
- Smoking
- Low consumption of fruits and vegetables
- Obesity
- Lack of exercise
- Exposure to blue and ultraviolet light
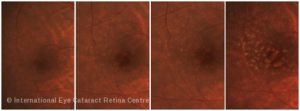
There are two types of AMD, commonly known as dry AMD and wet AMD. Dry AMD is also known as non-exudative or non-neovascular AMD while wet AMD is also termed exudative or neovascular AMD.
Dry AMD
The dry form of AMD is more common than the wet form, and accounts for about 90% of all cases of AMD. It develops very slowly and is characterised by cell deaths and thinning of the tissues in the macula.
One rare form of dry AMD, called geographic atrophy, causes severe vision loss through deaths of vital cells in the macula.
Wet AMD
Wet AMD is less common, and accounts for about 10% of all cases of AMD. However, it poses a much greater threat to central vision, and accounts for about 90% of severe vision loss from AMD.
In the early stages, abnormal new blood vessels grow underneath the macula and leak fluid and blood, causing disturbance to the central vision. Later, the light-sensitive retinal cells (photoreceptors) degenerate and scar tissue forms in the macula. This causes a blind spot in the centre of the vision, resulting in poor visual acuity.
AMD affects mainly the central vision and its effects range from no noticeable visual loss to mild vision loss and central blindness. AMD does not cause pain or redness of the eye.
Dry AMD
- Usually gradual onset
- Mostly no or mild visual symptom
- Slightly blurred vision or a blurry spot in the centre of the vision in the more severely affected eye
- Requires more light for reading and other visual tasks
Wet AMD
- Often sudden onset
- Blurred or fuzzy vision
- Straight lines appear wavy or distorted
- A dark or “empty” patch may appear in the centre of the vision
AMD is usually diagnosed during a retinal examination by an eye or retinal specialist. It can also be diagnosed by taking a colour photograph of the retina using a special camera (retinal photography).
A number of specialised tests such as Serial Colour Retinal Photography, Fundus Autofluorescence Imaging, High-definition Optical Coherence Tomography (OCT), Fundus Fluorescein Angiography (FFA) and Indocyanine Green (ICG) Angiography can help your retinal specialist evaluate and manage AMD better.
There is currently no definitive cure for AMD. However, early detection and treatment can help to prevent vision loss from AMD.
Dry AMD
There is currently no treatment that can reverse dry AMD. However, this does not mean that one is likely to become blind from dry AMD. Vision loss, when it occurs, is usually very gradual and mild in dry AMD. Most people with dry AMD are able to lead a normal and active lifestyle.
Patients with moderate or severe dry AMD should take high-dose vitamins (antioxidants) and zinc daily to reduce the likelihood of the condition progressing to advanced AMD. The Age-Related Eye Disease Study (AREDS), a multicentre clinical trial in the USA, has shown that taking such nutritional supplements daily can reduce the risk of developing advanced AMD by as much as 25% over 5 years. This was accompanied by a 19% reduction in the risk of moderate vision loss after 5 years.
Although there is no cure for wet AMD, there are treatments that can stop the growth of abnormal blood vessels and reduce macular swelling caused by AMD. Treatment may improve or restore vision in some cases or prevent further vision loss in others. However, in a few patients, the vision continues to deteriorate despite treatment.
Anti-Vascular Endothelial Growth Factor Therapy
A chemical called vascular endothelial growth factor (VEGF) has been shown to be critical in causing abnormal blood vessels to grow under the retina and to leak. Drugs that can block this trouble-causing VEGF have therefore been developed to treat AMD. These drugs, known as anti-VEGFs, help block the growth of abnormal blood vessels, slow their leakage and reduce vision loss.
Anti-VEGF drugs such as Lucentis (ranibizumab) and Eylea(aflibercept) are used.
Another anti-VEGF drug called Avastin (bevacizumab) has been approved for the treatment of colon cancer but not for wet AMD or to be used in the eye. Some doctors, however, use Avastin to treat wet AMD (called off-label treatment) to save cost.
Typically, patients receive multiple anti-VEGF injections over the course of many months. Some patients are given an injection every month for the first 3 months and the response to treatment closely monitored. Depending on the response to treatment, the eye may be further monitored for relapse of the condition and additional injections may be necessary.
There is a small risk of complications with anti-VEGF treatment, usually resulting from the injection itself, such as bleeding, retinal tear, retinal detachment, cataract formation and infection. For most patients, the benefits of this treatment outweigh the small risk of complications.
Anti-VEGF therapy is currently the most advanced treatment for wet AMD because they target the underlying cause of abnormal blood vessel growth and achieve the best possible outcome among currently available treatment methods. Although not every patient benefits from anti-VEGF treatment, a large majority of patients achieve stable vision and a significant percentage can improve their vision to some degree.

Photodynamic Therapy or Visudyne Therapy
Photodynamic therapy (PDT) involves the use of a light-sensitive drug called Visudyne (verteporfin) that is slowly infused into the bloodstream through a vein on the back of the hand. The drug travels in the bloodstream to the eye and, after a short interval, is absorbed by the abnormal blood vessels in the macula. Following this, a low-energy “cold” laser is shone onto the affected area of the macula for 83 seconds. This laser activates the drug which then causes a chemical reaction that help seals the abnormal blood vessels. Repeat treatment may be necessary in some cases when the abnormal blood vessels regrow.
Laser Photocoagulation
A very small number of patients with wet AMD have abnormal blood vessels that lie outside the centre of the macula. These patients may be treated with laser photocoagulation or “hot” laser. This involves directing a very intense light beam (laser) at the abnormal blood vessels to destroy them. The laser beam unfortunately also destroys the retina overlying the abnormal blood vessels. If the abnormal blood vessels are outside the centre of the macula, good central vision can be preserved because the centre of the macula is not affected by the laser. On the other hand, if the abnormal blood vessels are at the centre of the macula, laser treatment will affect the central vision. For this reason, laser photocoagulation is not performed for patients with abnormal blood vessels affecting the centre of the macula. Even for those who are suitable, recurrence of the abnormal vessels may develop after laser treatment and repeat treatment may be necessary.

Although AMD affects the macula and causes poor central vision, the peripheral retina is usually spared and side vision is retained. Affected individuals therefore do not become completely blind. High-intensity reading lamps and low vision aids such as magnifiers and closed-circuit televisions can help those affected make the most of their remaining vision. With the help of low vision aids, many patients continue to enjoy many of their favourite activities (eg, reading) and lead independent lives.
